Part 12: Resuscitation Education Science
Abstract
Developed by the American Heart Association, these Guidelines represent the first comprehensive update of education recommendations since 2020. Incorporating the results of structured evidence reviews from the International Liaison Committee on Resuscitation, these are guidelines for the design and delivery of resuscitation training for health care professionals and lay rescuers. This update emphasizes the continuous evolution of evidence evaluation and the necessity of adapting educational strategies to local needs and diverse community demographics. Existing guidelines remain relevant unless specifically updated in this publication. Key topics that are new, are substantially revised, or have significant new literature include the use of cardiopulmonary resuscitation feedback devices in training, rapid-cycle deliberate practice, teamwork and leadership training, manikin fidelity, gamified learning, virtual and augmented reality, use of cognitive aids, stepwise training, blended learning, scripted debriefing, instructor training, alternative objects for lay rescuer chest compression training, and special considerations for training in the management of opioid overdose. How certain personal considerations may influence the overall impact of education are also reviewed, including disparities accordingly related to gender, race, socioeconomic status, and language; the impact of training for school children; and factors that act as barriers or facilitators to lay rescuer willingness to perform cardiopulmonary resuscitation. We conclude with a summary of current knowledge gaps in resuscitation education science and a discussion of future directions for optimizing the impact of resuscitation training programs.
Top 10 Take-Home Messages
- Effective resuscitation education for lay rescuers and health care professionals is an essential component of the formula for survival from cardiac arrest.
- The use of cardiopulmonary resuscitation (CPR) feedback devices leads to improved skill performance and is recommended during skill training for lay rescuers and health care professionals.
- Disparities in public awareness, knowledge, and access to CPR education affect specific populations differently. It is recommended to focus efforts on public awareness campaigns and training availability in areas where these discrepancies are greatest.
- Children 12 years of age and older should be taught to perform effective CPR and defibrillation; children younger than 12 years of age should be trained in emergency response and CPR to improve confidence and willingness when they are older.
- Virtual reality (VR) and augmented reality (AR) can increase realism during resuscitation training. However, while VR can improve knowledge acquisition, AR should not be used to teach CPR skills.
- Gamified learning has been shown to improve learner engagement and enhance knowledge acquisition.
- The use of a script to guide debriefing during resuscitation training can help instructors by guiding discussions and enhancing consistency.
- Rapid-cycle deliberate practice (RCDP) during CPR training can lead to better skill performance after training.
- Alternative objects (eg, a pillow) have been studied as an inexpensive and accessible alternative to manikins for chest compression training, but more data is needed to determine their effectiveness.
- Goals for future research in resuscitation education include studies demonstrating impact on clinical outcomes, cost-effectiveness of instructional design elements, and improvement in the uniformity and quality of outcome measures across studies.
Preamble
Every year, millions of health care professionals and thousands of laypeople undergo basic life support (BLS) and advanced life support (ALS) training, aiming to improve patient outcomes in cases of cardiac arrest. Resuscitation training programs integrate evidence-based content with the opportunity to practice critical lifesaving skills in both individual and team-based clinical settings. While such training is widespread, it often falls short in achieving optimal performance for various reasons, with learners struggling to consistently apply acquired skills in public/out-of-hospital events as well as in patient care.1,2
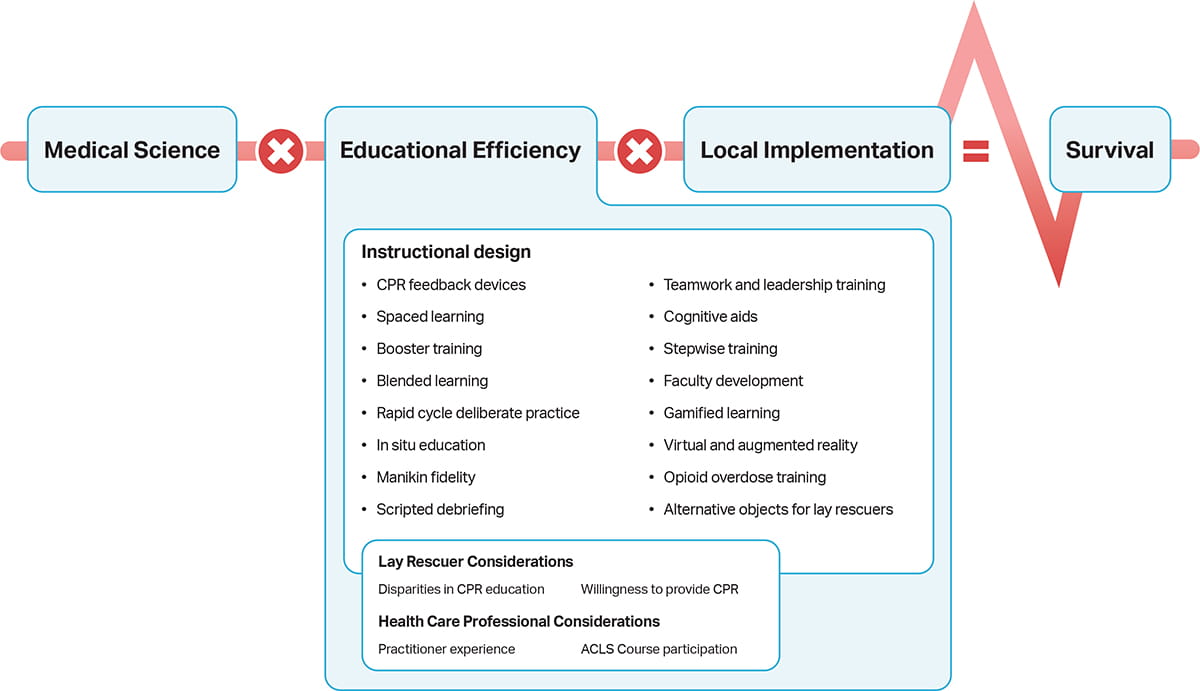
The International Liaison Committee on Resuscitation (ILCOR) Formula for Survival (Figure) emphasizes 3 essential components influencing survival outcomes from cardiac arrest: guidelines based on current resuscitation science, effective education of lay rescuers and health care professionals, and local implementation of guidelines.3 The provision of an effective education component is highly dependent on the instructional design of the educational endeavor because design strongly determines how content is delivered to and ultimately taken up by the learner. Placing greater emphasis on our understanding of how to increase the effectiveness of education programs will improve performance and lay rescuer confidence and enhance local implementation, all of which lead to the ultimate goal of increasing survival from sudden cardiac arrest.
These Guidelines contain recommendations for the design and delivery of resuscitation training for both lay rescuers and health care professionals. In Part 12, we explore the evidence informing different instructional design features and discuss how factors related to individuals, both lay rescuers and health care professionals, may influence CPR training, willingness to perform CPR, and quality of CPR performance.
Scope of the Guidelines
Cardiac arrest remains a major public health problem, with more than 600 000 cardiac arrests per year in the United States, both in and outside the hospital.1,2 Survival rates of patients who experience cardiac arrest remain low despite significant advancements in resuscitation science and treatment; however, it is clear that timely CPR and use of an automated external defibrillator (AED) can double survival.3 Each year, millions of people receive BLS and ALS training in an effort to improve the quality of CPR delivered to people experiencing cardiac arrest.4 Resuscitation training programs are designed to convey evidence-based content and provide opportunities for learners (ie, those enrolled in resuscitation training programs) to apply knowledge and practice critical skills. These programs, however, frequently fall short of achieving the desired learning outcomes (eg, knowledge and skill acquisition), with performance that does not consistently translate over to real-world environments.4,5 For example, CPR skills that are acquired immediately after BLS training often show decay by as early as 3 months, resulting in many BLS-trained lay rescuers and health care professionals—such as physicians, nurses, respiratory therapists, and emergency medical responders—challenged to perform Guideline-compliant CPR during simulated and real cardiac arrests.6-14 Additionally, current research on lay rescuer CPR (LR-CPR) training lacks evidence describing how to train lay rescuers to consistently recognize cardiac arrest, initiate CPR, and use AEDs appropriately.15-17 A dedicated focus on instructional design rooted in human psychology and behavior and learning science is essential to ensure that knowledge and skills acquired during training are easily and habitually applied in real-life cardiac arrest.4
Improving survival from cardiac arrest is highly dependent on the quality and timeliness of resuscitative care. Many key determinants of a higher chance of survival, such as immediate recognition of cardiac arrest, early initiation of CPR, early defibrillation, and high-quality chest compressions, are variables that can be targeted by resuscitation training programs. Instructional design features are the key elements, or “active ingredients,” of resuscitation training programs that determine how content is delivered to the learner.18 A better understanding of the impact of instructional design features, including the effectiveness of training aids, on learning outcomes will enable educators to design training programs that translate into outstanding skill performance during cardiac arrests. Furthermore, appreciating how social determinants of health (eg, SES, race) and individual factors (eg, practitioner experience) influence the impact of resuscitation education will help inform future policy and implementation strategies. In this Part, we describe the evidence supporting key elements of resuscitation education and provide recommendations aimed at improving learner outcomes and patient outcomes from cardiac arrest. The following sections briefly describe the process of evidence review and guideline development. See “Part 2: Evidence Evaluation and Guidelines Development” in the 2025 American Heart Association (AHA) Guidelines for CPR and Emergency Cardiovascular Care (ECC) for more details on this process.
Organization of the Resuscitation Education Science Writing Group
The Resuscitation Education Science Writing Group comprised a diverse team of experts with backgrounds in resuscitation education, clinical medicine (ie, pediatrics, intensive care, emergency medicine), nursing, prehospital care, health services, and education research. Writing group members are AHA volunteers with an interest and recognized expertise in resuscitation and are selected by the AHA ECC Committee. The AHA has rigorous conflict-of-interest policies and procedures to minimize the risk of bias and improper influence during development of the Guidelines.19 Before appointment, writing group members and peer reviewers disclosed all commercial relationships and other potential (including intellectual) conflicts. Disclosure information for writing group members are listed in Appendix 1(link opens in new window).
Methodology and Evidence Review
Part 12 of the 2025 Guidelines is based on the extensive evidence evaluation performed in conjunction with ILCOR and affiliated ILCOR member councils. Four different types of evidence reviews (systematic reviews, scoping reviews, evidence updates, and writing group evidence evaluations) were used in the 2025 process. Each of these resulted in a description of the literature that facilitated Guideline development.20-24
Class of Recommendation and Level of Evidence
The AHA Resuscitation Education Science Writing Group reviewed all relevant and current AHA Guidelines for CPR and ECC5,25-35 and the relevant ILCOR Consensus on Science With Treatment Recommendations27 to determine if current guidelines should be reaffirmed, revised, or retired and whether new recommendations were needed. The writing group then drafted, reviewed, and approved recommendations, assigning to each a Level of Evidence (LOE; ie, quality) and Class of Recommendation (COR; ie, strength) (Table 1).
Importantly, applying Grading of Recommendations Assessment, Development, and Evaluation36 to educational studies yields greater challenges than its application to clinical studies. Specific considerations for studies involving educational outcomes (eg, improved outcomes in simulated patient settings or improved performance on summative assessment tools) are not provided in Grading of Recommendations Assessment, Development, and Evaluation methodology; instead, the writing group frequently assigned LOE to these studies according to a combination of a typical review of study quality, perceived importance of underlying constructs in the context of educational science, and, where possible, extrapolation of findings to analogous clinical phenomena (eg, outcomes in real patients as opposed to simulated ones).
Open table in a new window.
Guideline Structure
The 2025 Guidelines are organized into knowledge chunks grouped into discrete modules of information on specific topics or management issues.37 Each modular knowledge chunk includes a table of recommendations using standard AHA nomenclature of COR and LOE. A brief introduction or short synopsis puts the recommendations into context with important background information and overarching management or treatment concepts. Recommendation-specific supportive text clarifies the rationale and key study data supporting the recommendations. Hyperlinked references are provided to facilitate quick access and review.
Document Review and Approval
These Guidelines were submitted for blinded peer review to subject matter experts nominated by the AHA. Peer reviewer feedback was provided for the Guidelines in draft format and again in final format. The Guidelines were reviewed and approved for publication by the AHA Science Advisory and Coordinating Committee and the AHA Executive Committee. Disclosure information for peer reviewers is listed in Appendix 2(link opens in new window).
Major Concepts
This Part is divided into 3 main sections: (a) instructional design and aids, (b) individual learner considerations, and (c) knowledge gaps and future research. Instructional design refers to the way in which curricula are designed and structured to help learners meet their objectives. When optimally implemented, instructional design involves recognizing the needs and contexts of individual learners and aligning the objectives of a given curriculum to best meet those needs.1-3 Instructional design features take many forms, including features related to content (eg, team training), manikins or equipment (eg, manikin fidelity), methods of content delivery (eg, blended learning, spaced practice, RCDP), methods of content presentation (eg, VR, gamified learning), and other aspects of instruction. Resuscitation training programs may incorporate a key instructional design feature, or multiple features may be blended in an effort to optimize learning outcomes. In the first section, we offer recommendations related to the use of CPR feedback devices during training, RCDP, spaced learning and booster training, teamwork training, in situ training, levels of manikin fidelity, use of cognitive aids, gamified learning, VR and AR, blended learning, stepwise learning, scripted debriefing, and lay rescuer training in the management of opioid overdose.
In the second section, we describe how certain learner considerations may influence the overall impact of education. These include disparities related to gender, race, SES, and language; training of school-age children; as well as factors that act as barriers or facilitators to lay rescuer willingness to perform CPR. All of these considerations feed into the potential impact of instructional design and ultimately influence the educational efficiency component of the Formula for Survival (Figure).4
We conclude Part 12 of the 2025 Guidelines with a summary of current systematic shortcomings in resuscitation education research, a discussion of knowledge gaps in resuscitation education science, and future directions for optimizing the impact of resuscitation training programs.
| COR | LOE | Recommendations |
|---|---|---|
| 1 | A | 1. Feedback devices are recommended for use during CPR training for health care professionals. |
| 1 | A | 2. Feedback devices are recommended for use during CPR training for lay rescuers. |
Synopsis
Accurate and reliable feedback is crucial for enabling learners to improve their performance. Prior studies demonstrate that visual assessment of CPR quality is often unreliable,1,2 making it challenging for instructors to consistently deliver accurate feedback during training. Feedback devices for CPR help overcome this limitation by providing objective, real-time data to learners during training. Recent scientific statements have emphasized the importance of using CPR feedback devices during resuscitation training.3 While earlier reviews indicate that these devices can enhance short-term educational outcomes,4 there is a scarcity of studies objectively assessing CPR quality after training. No studies reported on cost-effectiveness, quality of CPR during real resuscitation, or patient survival.
Recommendation-Specific Supportive Text
- Seventeen randomized controlled trials (RCTs) assessed the impact of using feedback devices during training on the quality of CPR compressions performed by health care professionals.5-21 The meta-analyses demonstrated that CPR feedback devices had a moderate to large effect on all CPR quality metrics. Specifically, the use of feedback devices significantly increases mean compression depth, reduces deviations from the guideline-compliant compression rate, and improves compression depth, rate, and recoil compliance.
- Three RCTs22-24 conducted with lay responders demonstrated that feedback devices were effective in increasing mean compression depth,22,23 improving compression depth,22-24 and rate compliance,22 and reducing deviations from the Guidelines for mean compression rate.22-24 The effect on recoil compliance was not statistically significant in lay rescuers.22,23
| COR | LOE | Recommendations |
|---|---|---|
| 1 | B-R | 1. It is recommended to implement booster sessions when utilizing a massed learning approach for resuscitation training. |
| 2a | B-R | 2. It is reasonable to use an spaced learning approach in place of a massed learning approach for resuscitation training. |
Synopsis
Traditional resuscitation courses typically follow a massed learning approach, consisting of a single training event that lasts several hours or days, with retraining occurring every 1 to 2 years.1 In contrast, some resuscitation courses adopt a spaced learning approach, where training is divided into multiple sessions lasting from minutes to hours, dispersed weeks or months apart.2-5 Each session in a spaced learning format either introduces new content or reinforces material from previous sessions. Another instructional strategy is booster training, which involves brief weekly or monthly sessions designed to reinforce content initially taught in a massed learning course.6-19
For advanced pediatric resuscitation training, spaced learning courses have been found to be at least as effective or more effective than massed learning courses.3-5 No studies have directly compared spaced learning with massed learning for BLS, neonatal resuscitation (eg, the Neonatal Resuscitation Program), or advanced cardiovascular life support (ACLS) courses. Frequent booster training sessions conducted at 1- to 6-month intervals 6-12 as well as implementation of weekly booster sessions for Neonatal Resuscitation Program training reduced infant mortality.13 However, a study found increased booster frequency reduced attendance rates, with the highest attrition.6 No studies have evaluated booster training for pediatric advanced life support or ACLS courses.
Recommendation-Specific Supportive Text
- Seven RCTs compared booster CPR training at intervals of 1 to 6 months with no booster training.6-12 In 1 RCT, nurses who received more frequent CPR booster training showed a dose-dependent improvement in 1-year CPR skills. The proportion of participants achieving excellent CPR at 12 months was highest in those receiving monthly boosters.6 Another RCT found that emergency department professionals who received monthly booster training had higher rates of excellent 12-month CPR performance compared to those who received no boosters.7 One study reported improvements in CPR knowledge and skills following 30-minute booster sessions at 1, 3, and 6 months.8 Another found enhanced ventilation and compression quality after monthly booster sessions.9,10 One study observed shorter times to chest compressions and defibrillation following 15-minute booster sessions administered every 2, 3, or 6 months.11 A lay rescuer study found every 6-month booster training demonstrated better CPR skill retention.14 For neonatal resuscitation, 3 RCTs indicated that more frequent Neonatal Resuscitation Program booster sessions (ranging from weekly to 9 months) were associated with sustained improvements in skill performance.15,16,18 One observational study reported both improved clinical performance and reduced infant mortality following implementation of 3- to 5-minute weekly booster sessions.13
- Two RCTs and 1 observational study have compared spaced learning with massed learning for pediatric resuscitation training.3-5 In 1 RCT, emergency medical services (EMS) professionals were randomized to either a spaced learning format (4 weekly sessions) or a massed learning format (2 consecutive days).3 At 3 months, the spaced learning group demonstrated superior retention of infant bag-mask ventilation and infant intraosseous insertion skills compared to the massed learning group; no significant difference was observed in chest compression skills. Additionally, knowledge decay was noted in the massed learning group but not in the spaced learning group.3 In another RCT, pediatric nurses and respiratory therapists were assigned to either a spaced learning approach (6 sessions over 6 months) or a massed learning format (a single day) for pediatric advanced life support recertification.4 Clinical performance scores improved in the spaced learning group, while both groups showed similar improvements in teamwork at course completion. An observational study examined medical students who completed pediatric resuscitation training through either a spaced learning format (4 weekly sessions) or a massed learning session (a single session).5 At 4 weeks after training, no significant differences were found between the groups in knowledge or skills.
| COR | LOE | Recommendations |
|---|---|---|
| 2b | C-LD | 1. It may be reasonable to incorporate RCDP as part of BLS or ALS training for health care personnel. |
Synopsis
Rapid-cycle deliberate practice is a simulation-based training method that incorporates within-event debriefing.1,2 RCDP is defined by rapid cycling between deliberate practice and directed feedback until skill mastery is achieved.3 In simulations incorporating RCDP, the scenario is stopped at specific points (eg, time-outs), during which the facilitator gives learners feedback on performance. After the pause, the simulation is restarted and allowed to continue until another pause. Thus, the debriefing in RCDP is done in small chunks during the scenario and not after the scenario is completed. By the end of an RCDP session, learners have repeated several steps of the scenario multiple times. RCDP typically occurs in the context of a single learning session and thus can be incorporated into BLS and ALS courses.
Several randomized and nonrandomized studies with very low quality of evidence involving predominantly trainees incorporated RCDP as part of BLS or ALS training.3-10 Knowledge gaps exist regarding the use of RCDP in lay rescuers and experienced health care professionals, the long-term impact of RCDP training, and the resources required to implement RCDP into life support training. Further research is needed to examine the effects of RCDP on clinical outcomes and patient survival.
Recommendation-Specific Supportive Text
- One randomized7 and 1 observational3 study found that time to chest compressions was faster in the RCDP groups. Two studies reported higher compression fractions in the RCDP groups.3,10 Studies show that the time to ventilate,3,6 to deliver a shock,3,7,10 and to the administration of epinephrine6 were all shorter in the RCDP groups. Two studies found that RCDP groups had better odds of performing defibrillation within 2 and 3 minutes.3,4 Two studies found that defibrillation before pause was significantly shorter in RCDP groups.3,10 One randomized study showed lower NASA Task Load Index workload scores in RCDP participants compared to controls.7 One study reported differences in teaching effectiveness as reported by learners in favor of controls.5
| COR | LOE | Recommendations |
|---|---|---|
| 1 | B-R | 1. It is recommended that life support training for health care professionals includes a specific emphasis on teamwork competencies. |
Synopsis
Lapses in teamwork are a major contributor to unintended harm across health care.1 Cardiac arrest outcomes are dependent on effective teamwork, given the need for the simultaneous delivery of several time-sensitive interventions.2-4 Thus, in addition to training focusing on technical skills such as delivering high-quality CPR, life support training commonly includes training specifically targeting teamwork competencies including communication, leadership, decision-making, and workload management. The addition of teamwork training to life support courses may represent an opportunity to enhance patient safety.
Recommendation-Specific Supportive Text
- Sixteen studies (14 RCTs and 2 observational studies) examined the impact of a specific emphasis on teamwork competencies in life support training on teamwork performance measures. Twelve of 14 RCTs demonstrated superior performance after specific teamwork training in outcomes related to communication,1-7 leadership behavior,4,8,9 nontechnical skills,10,11 workload management,6,7 and overall teamwork12 at course completion. One observational study13 reported higher scores on overall teamwork measures, while the other14 found no difference in teamwork or leadership measures. Two5,12 of the 35,12,15 RCTs reporting outcomes beyond course completion demonstrated improvement in teamwork measures.
Thirteen studies, 12 RCTs, and 1 observational study examined the impact of teamwork training on the performance of various technical skills such as adherence to guidelines,3 time to specific behaviors,5,6,10,11,13 completion of tasks such as intubation or medication administration,8,11-13,15-17 or CPR quality parameters,2-5,8 Of these 13 studies, 7 demonstrated improvement in at least one measure of technical skills performance either at2,3,10,11,13 or beyond course completion.5,12
| COR | LOE | Recommendations |
|---|---|---|
| 2b | C-LD | 1. It may be reasonable to use gamified learning elements as a component of resuscitation training for health care professionals. |
| 2b | C-LD | 1. It may be reasonable to use gamified learning elements as a component of CPR instruction for lay rescuers. |
Synopsis
Gamified learning involves the use of game-like elements during resuscitation training. These elements can include competition, point systems, scaffolded levels of difficulty, and leaderboards. Gamified learning has been shown to increase learner engagement and enhance recall of content.1 Gamified learning elements, both digital and nondigital, have been included in resuscitation training in an effort to create a greater degree of stimulation and engagement using active participation with and alongside peers, particularly for younger generations.
Significant heterogeneity exists in the literature regarding definitions of gamification, learning platforms, and assessment methods and metrics. More robust data are needed regarding generalizability and implementation, as well as understanding learner responses to gamification and possible patient outcomes.
Recommendation-Specific Supportive Text
- Eleven studies in health care professionals evaluated outcomes of CPR skill performance, knowledge, and attitudes. One RCT using an online competitive platform showed improved CPR performance,2 but multiple studies using leaderboards to monitor competition showed mixed results.3,4 One RCT comparing smartphone-based games before and during the ALS course to no gaming showed no difference in ALS skills.5 In contrast, an online gaming portal improved neonatal resuscitation scores in an observational study.6 Multiple observational and RCT studies showed improved knowledge scores following a board game, a point-based screen game, a leaderboard, and smartphone-based games.2,5,7,8 Self-reported confidence was higher among smartphone-based game users than nonusers5 and players of a card game designed for neonatal resuscitation knowledge training reported high levels of perceived usefulness following the training.9 Overall, for health care professionals, the evidence suggests that gamified learning was associated with improved CPR skill performance, knowledge, and self-confidence; however, because of low quality and heterogeneity among these studies, the recommendation remains weak.
- Two studies in high school students examined CPR skill following a CPR tournament or a screen-based competition. Both studies showed immediate and 3-month to 6-month post training improvement in CPR skills compared with baseline or control group.10,11 No studies evaluated CPR knowledge as an outcome. One RCT of a screen-based competition compared to standard training reported a higher proportion of learners in the competition group feeling emotions reported by lay rescuers such as afraid, nervous, or upset.11 For laypersons, the evidence suggests gamified learning was associated with improved CPR skill performance and an emotional response similar to actual lay rescuers. Because of low quality and heterogeneity among these studies, the recommendation remains weak.
| COR | LOE | Recommendations |
|---|---|---|
| 2b | B-R | 1. It may be reasonable to use VR to support knowledge acquisition in BLS and ALS training for lay rescuers and health care professionals. |
| 2b | C-LD | 2. The use of AR to provide real-time CPR feedback may be considered for BLS training of lay rescuers and health care professionals. |
| 3: Harm | B-R | 3. VR should not be used for CPR skill acquisition in lay rescuers and health care professionals. |
Synopsis
Gamified learning involves the use of game-like elements during resuscitation training. These elements can include competition, point systems, scaffolded levels of difficulty, and leaderboards. Gamified learning has been shown to increase learner engagement and enhance recall of content.1 Gamified learning elements, both digital and nondigital, have been included in resuscitation training in an effort to create a greater degree of stimulation and engagement using active participation with and alongside peers, particularly for younger generations.
Significant heterogeneity exists in the literature regarding definitions of gamification, learning platforms, and assessment methods and metrics. More robust data are needed regarding generalizability and implementation, as well as understanding learner responses to gamification and possible patient outcomes.
Recommendation-Specific Supportive Text
- Eleven studies in health care professionals evaluated outcomes of CPR skill performance, knowledge, and attitudes. One RCT using an online competitive platform showed improved CPR performance,2 but multiple studies using leaderboards to monitor competition showed mixed results.3,4 One RCT comparing smartphone-based games before and during the ALS course to no gaming showed no difference in ALS skills.5 In contrast, an online gaming portal improved neonatal resuscitation scores in an observational study.6 Multiple observational and RCT studies showed improved knowledge scores following a board game, a point-based screen game, a leaderboard, and smartphone-based games.2,5,7,8 Self-reported confidence was higher among smartphone-based game users than nonusers5 and players of a card game designed for neonatal resuscitation knowledge training reported high levels of perceived usefulness following the training.9 Overall, for health care professionals, the evidence suggests that gamified learning was associated with improved CPR skill performance, knowledge, and self-confidence; however, because of low quality and heterogeneity among these studies, the recommendation remains weak.
- Two studies in high school students examined CPR skill following a CPR tournament or a screen-based competition. Both studies showed immediate and 3-month to 6-month posttraining improvement in CPR skills compared with baseline or control group.10,11 No studies evaluated CPR knowledge as an outcome. One RCT of a screen-based competition compared to standard training reported a higher proportion of learners in the competition group feeling emotions reported by lay rescuers such as afraid, nervous, or upset.11 For laypersons, the evidence suggests gamified learning was associated with improved CPR skill performance and an emotional response similar to actual lay rescuers. Because of low quality and heterogeneity among these studies, the recommendation remains weak.
| COR | LOE | Recommendations |
|---|---|---|
| 2b | B-R | 1. The use of higher-fidelity manikins for BLS and ALS training can be beneficial for learners in training settings with available infrastructure. |
| 2b | C-LD | 2. The use of lower-fidelity manikins during BLS and ALS training may be considered in training settings where higher-fidelity manikins cannot be used for any reason. |
| 2b | C-EO | 3. It may be reasonable for instructors to use manikins and manikin features in a manner that allows for alignment of learning objectives to the specific needs of learners. |
Synopsis
The term fidelity is used to describe features in a simulation setting that improve realism and allow learners to suspend disbelief to a greater extent. When the term fidelity is applied to manikins, it refers to the presence of physical features (visible, audible, palpable, etc.) and physiologic responses that make the manikin more closely resemble an actual patient. This increased physical realism may theoretically lead to greater engagement of learners, with the goal of improving educational outcomes. Limitations to higher-fidelity manikin use include high costs, availability of personnel and infrastructure to operate and maintain them (eg, technological resources), and limitations to manikin design in terms of physical features and their optimal applicability to learning objectives.1,2 Data are lacking comparing manikin fidelity on patient outcomes and the effects of fidelity level on lay rescuer training.
Recommendation-Specific Supportive Text
- A meta-analysis of 8 RCTs examining the effect of higher manikin fidelity on learning outcomes found modest improvement in psychomotor skill performance during immediate post-training assessment using simulated clinical scenarios. Another meta-analysis of 7 RCTs found no impact of manikin fidelity on immediate post training knowledge assessment.3 Three RCTs examined teamwork performance between groups trained on higher- versus lower-fidelity manikins; 2 of the RCTs found positive effect of higher fidelity, while one found no difference.4-6 Three RCTs examined psychomotor skill at 3 months or greater after training with mixed results.7-9 Three RCTs examined knowledge at 6 months or longer after training based on higher- versus lower-fidelity manikin use, with mixed results.7,9,10 Two studies reported exclusively on learner satisfaction and confidence; both demonstrated high levels of positive responses from learners.11,12
- In a recent systematic review, 4 RCTs comparing higher- versus lower-fidelity manikins found no significant difference in learning outcomes across a variety of life support curricula, while at the same time demonstrating that both high- and low-fidelity manikins resulted in significant improvement in skill or knowledge compared to a pretraining baseline assessment.4,13-15
- Because physical features of manikins vary, it may be reasonable for instructors to train learners using manikins and manikin features that are optimally realistic based on the learning objectives of a given training session (eg, manikin with compressible chest wall for CPR training).1,2
| COR | LOE | Recommendations |
|---|---|---|
| 2a | C-LD | 1. It may be reasonable for health care professionals to use cognitive aids during resuscitation. |
| 3: No Benefit | C-LD | 2. It is not recommended for lay rescuers to use cognitive aids during resuscitation.1-10 |
Synopsis
Cognitive aids are resources that provide prompts aimed to encourage recall of information and increase the likelihood of correct performance/behaviors. Cognitive aids can be divided into interactive (bidirectional flow of data, eg, digital app) or noninteractive (unidirectional flow of data, eg, algorithm card). There is significant heterogeneity in the literature in terms of study design, cognitive aid tool (eg, checklist, mobile device app, voice prompts, or pictures/flowsheet), and assessment methods/metrics. Published simulation data suggests that cognitive aid use by health care professionals and lay rescuers during resuscitation efforts have different impacts on the effectiveness of the resuscitation process, leading to opposing recommendations for these different groups.
Recommendation-Specific Supportive Text
- Nineteen small simulation-based studies in health care professionals (physicians, nurses, multidisciplinary teams, and medical students) evaluated the outcomes of CPR quality, and adherence to protocols/process during resuscitation. For CPR quality, 1 RCT of noninteractive cognitive aid showed improved chest compression quality,1 1 RCT of interactive cognitive aid showed improved CPR performance score,2 and 1 RCT showed no difference.3 Studies of interactive cognitive aids included 4 non-RCTs4-7 and 6 RCTs8-14 showing improved adherence to protocol or procedure compared to controls. Two RCTs of noninteractive cognitive aids showed no difference in protocol adherence compared to control,15,16 and 3 RCTs showed improved protocol adherence.17-19 Overall, for health care professionals the evidence suggests that use of cognitive aids during simulated resuscitation efforts may lead to improved adherence to protocols and may improve CPR quality.
- Ten small simulation-based studies in lay rescuers evaluated the outcomes of CPR quality and adherence to protocol/process during simulated resuscitation. For the outcome of CPR quality, 1 RCT using a noninteractive flowchart showed reduced hands-off time during CPR,20 1 RCT using a noninteractive smartphone app improved compression rate and depth,21 and 1 RCT using an interactive cognitive aid showed improved adherence to 30:2 CPR ratio.22 One observational study using chatbot guidance described low rates of high-quality CPR achieved, but had no comparison group.23 One RCT comparing various-length noninteractive checklists showed no difference in CPR quality.24 For the outcome of adherence to protocol/process, 3 RCTs (both interactive and noninteractive cognitive aids) showed improved adherence,21,25,26 1 RCT of noninteractive s showed no improvement,27 and 1 RCT and 1 observational study of noninteractive cognitive aids showed improved adherence to protocol.28,29 However, 2 RCT of interactive20,22 and one RCT of noninteractive cognitive aids26 showed significant delays (30–70 seconds) in calling emergency services and initiating chest compressions. Although studies demonstrated some improved CPR quality, this is outweighed by the statistically significant and clinically relevant delays to critical actions in the chain of survival.
| COR | LOE | Recommendations |
|---|---|---|
| 2b | C-LD | 1. It may be reasonable to use a stepwise approach for skills-teaching in resuscitation training. |
Synopsis
The ideal approaches for teaching resuscitation skills, considering learner performance, retention, confidence, and preference are not currently known and various stepwise approaches exist amongst courses developed by the world’s leading resuscitation organizations. A stepwise approach is a deliberate skills-teaching methodology, including 2 or more steps (eg, Halsted’s “see one, do one” approach). Stepwise approaches can vary considerably in number and order of steps, instructor/learner presence (eg,in-person or virtual),skills demonstration modality (eg, live versus prerecorded),and whether feedback is, or is not, provided by the instructor. Other stepwise approaches include Peyton’s 4-step approach, which uses well-defined serial steps including demonstration, deconstruction,comprehension, and learner performance and practice.
Recommendation-Specific Supportive Text
- Data primarily supported from a systematic review of 17 studies, including 14 RCTs1-17 and 3 non-RCTs.17-19 Skills were heterogeneous, ranging from very basic, such as nasogastric tube insertion8,10,to very advanced, such as endotracheal intubation and cricothyrotomy.6,18 Most studies assessed chest compressions,2,3,5,7,9,11,13,16,19 AED use,2,3,7 and basic airway management.2,3,5,7,11,14 The majority of studies included medical students1,5-10,13,14,16-19,2 studies included nursing students11,15,and 2 studies involved lay rescuers.2,3 Regarding end-of-course skills performance (up to 3 months after the course),only 2 studies demonstrated superiority utilizing Peyton’s stepwise approach.5,18 The remaining studies showed no differences between stepwise approaches versus non-stepwise approaches. Skills retention, reevaluated 2 to 3 months after the course, was unaffected by a stepwise approach.13,14,19 One study demonstrated significantly increased BLS/AED skill and confidence with live instructor-performed skills demonstration compared to recorded video demonstration.7 There was a trend toward learners preferring a stepwise approach, with 2 studies demonstrating higher overall learner satisfaction.1,18 Two studies showed no difference in learner preferences2,7; instructor preference was not analyzed in the studies.
| COR | LOE | Recommendations |
|---|---|---|
| 2a | C-LD | 1. It is reasonable to conduct in situ simulation-based resuscitation training in addition to traditional training. |
| 2b | B-R | 2. It may be reasonable to conduct in situ simulation-based resuscitation training in place of traditional training. |
Synopsis
In situ simulation refers to a subset of simulation activities occurring in actual patient care areas (ie, real clinical environment).1 In situ simulation can be used as a strategy to train individuals or health care teams.2,3 The objectives for in situ training can be individual technical skills or team-based skills, including communication, leadership, role allocation, and situational awareness.2,3 One distinct advantage of in situ training is that it provides learners with a more realistic training environment. We explored if in situ, simulation-based resuscitation training for health care professionals leads to improved learning, performance, and patient outcomes.
Studies comparing in situ training to traditional training (ie, classroom or laboratory-based training) have demonstrated mixed results in learning outcomes.4-7 Compared with no intervention, in situ training added to other educational strategies has a positive impact on learning outcomes (eg, improved team performance, improved time to critical tasks),8-15 performance change in the real clinical environment (eg, improved team performance, recognition of deteriorating patients),8,16,17 and patient outcomes (eg, improved survival, neurological outcomes).15,16,18-21
Recommendation-Specific Supportive Text
- Four observational studies demonstrated that regular in situ simulation training, in combination with or in addition to other educational strategies (ie, standard classroom training, refresher of BLS/pediatric advanced life support training, introduction of code teams, distributed practice), is effective at improving team performance, time to recognize deteriorating patients, and code documentation.8,16,17,22 Four additional observational studies assessing bundled interventions including in situ training demonstrated significant improvements in cardiac arrest survival.16,18-20 Because in situ training was tested as part of a bundled intervention in these studies, the individual contribution of in situ training cannot be clearly elucidated. Two RCTs demonstrated that in situ cardiac arrest training coupled with spaced learning yields better learning outcomes (ie, improved clinical performance, decreased time to initiate compressions and defibrillation) compared with training conducted in a massed-delivery format in the classroom.11,14 One RCT and 4 prospective observational studies demonstrated that in situ simulation training results in improved clinical performance in simulated environments.8-10,12,13 Two observational before-and-after studies of neonatal resuscitations found incorporating in situ simulations improved specific task performance (time to heart rate) and teamwork,15 as well as improved clinical outcomes.21 Most observational studies are limited by a lack of parallel control groups, a lack of performance measures with supportive validity evidence, and potential confounding factors.
- Three RCTs and 1 observational study compared learning outcomes (ie, team performance, technical skills) of in situ simulation training with standard classroom or laboratory-based training settings. One RCT demonstrated improved performance in the in situ group while the other studies demonstrated no significant differences between the 2 settings.4-7
| COR | LOE | Recommendations |
|---|---|---|
| 2b | C-LD | 1. It may be reasonable for an instructor to use a debriefing script during resuscitation education. |
Synopsis
Scripted debriefing involves the creation of a written plan for debriefing learners during or following life support training. It may include such elements as specified sets of topics or subtopics for the debriefing, suggested words or phrases to guide the discussion, and a framework to structure the debriefing. These scripts aim to standardize debriefing during resuscitation training, supporting facilitators with a clear plan and guiding discussion. Standardized debriefing helps to maintain consistency in the delivery of debriefings across training centers and resuscitation programs. Six studies were identified with varying outcomes.1-6 Despite the limited and mixed data, scripted debriefing holds significant potential to enhance CPR training. The integration of quantitative data, such as CPR quality, into debriefings is particularly promising. Further exploration is necessary as we integrate these principles into clinical event debriefings. Future research should concentrate on optimizing debriefing script designs to achieve the best learning outcomes across different learner groups.
Recommendation-Specific Supportive Text
- Six studies used simulation scenarios to evaluate scripted debriefing.1-6 A multicenter RCT with 453 health care professionals found scripted debriefing improved team leadership skills and knowledge acquisition but no difference in clinical performance.2 Another study found no difference in teamwork performance or learner satisfaction among medical and nursing students using scripted debriefing.3 In an RCT of 80 health care professionals, data-informed scripted debriefing improved CPR quality metrics, such as overall excellent CPR, depth, chest compression fraction, and perishock pause duration, but no difference in time to critical interventions, time to initiate CPR, time to first defibrillation, and time to the first dose of epinephrine.1 Another nonrandomized study found no significant difference in clinical judgment using scripted or nonscripted debriefing among nursing students.6 A multicenter, cluster-randomized trial with novice and expert instructors and 70 participants found scripted debriefings improved debriefing quality, especially for novice instructors, but not for experts.5 A single-center RCT found no difference in the debriefing quality of novice instructors when using a script.4 One RCT studying novice debriefers’ cognitive load and workload while debriefing trained actors in video-recorded simulated resuscitations using a debriefing script found reduced debriefer cognitive load in the scripted debriefing group but no difference in debriefer workload.4
| COR | LOE | Recommendations |
|---|---|---|
| 2b | B-NR | 1. A blended learning educational approach may be considered for teaching guideline-based life support courses. |
Synopsis
Blended learning combines traditional classroom instruction with electronic or online methods. Blended learning incorporates various attributes from 4 domains: communication synchronicity, location, delivery method, and educational philosophy. Traditional educational methods (eg, in-class learning) in resuscitation courses have transformed due to technological advancements, evidence-based educational science, and time and financial constraints for learners, faculty, and sponsoring organizations. Nontraditional education methodologies, including blended learning, have numerous advantages, which became more obvious during the COVID-19 pandemic, and have become widely implemented and adopted for the long term. This recommendation addresses whether blended learning, for lay rescuers and health care professionals taking an accredited life support course, affects knowledge, skill acquisition and retention, participant satisfaction, and resource outcomes.
Recommendation-Specific Supportive Text
- Data are primarily extracted from a systematic review encompassing 13 courses.1 In comparing blended learning to traditional courses, knowledge1-11 acquisition was mixed while skills acquisition studies2-4,6-10,12-19 predominantly found no differences, though a few showed blended learning superiority in various specific resuscitation skills.2,13,18,19 Knowledge retention consistently demonstrated no differences between blended learning and traditional courses.2-4,8 Skills retention was more variable, with 5 of the studies demonstrating no differences,3,4,14,15,17 and the remaining 4 studies10,11,3,5,19 reporting mixed findings.2,8,19 Learner satisfaction toward blended learning in BLS studies were equally split between those observing no differences9,17 and those demonstrating more favorable attitudes.19 Among ALS-based studies, 3 studies6,10,12 showed more favorable attitudes toward the blended learning approach while 2 studies3,5 demonstrated learner preference for traditional educational methods. Of the 4 studies (2 BLS and 2 ALS)6,11,23,24 evaluating costs, blended learning demonstrated long-term cost savings through fewer employment absences for learners and faculty, despite the initial higher set-up costs for Guideline-based life support courses.7,9,20
| COR | LOE | Recommendations |
|---|---|---|
| 1 | B-R | 1. Initial instructor training is recommended for individuals teaching BLS and ALS courses. |
| 2a | B-R | 2. Ongoing instructor development is reasonable for individuals teaching BLS and ALS courses. |
Synopsis
The educational effectiveness of life support courses is one of several factors that can enhance CPR quality. The effectiveness of CPR education is heavily dependent on the quality and ability of life support course instructors who are responsible for delivering both basic and advanced resuscitation courses. Many resuscitation training organizations have developed initial instructor training for instructor candidates and ongoing instructor development opportunities for current instructors. A 2018 AHA scientific statement on resuscitation education suggested a variety of approaches to improve the competency of life support course instructors.1 A 2022 ILCOR scoping review on faculty development identified 4 general themes to improve the quality and ability of life support course instructors, which included instructor qualification and training, assessment tools, teaching skill enhancement, and additional instructor courses.2
Recommendation-Specific Supportive Text
- Ten studies examined initial instructor training with heterogeneous outcomes of interest.1-10 Five studies used a train-the-trainer instructor course design and reported improvements in knowledge, comfort levels, and resuscitation skills after train-the-trainer participation.1-3,5,9 In a study of a systemwide instructor training course, instructor candidates had a high pass rate on theoretical and practical tests.7 Multiple studies examined instructor development with mixed results.6,11-21
- One RCT examining the impact of additional instructor training found students taught by trained instructors performed worse on 2 clinical examinations sections and teaching quality was rated worse.14 In an RCT where ALS instructors were taught to identify team leader errors, the intervention group found and documented more errors and made more correct grade assignments.15 Two studies examining the assessment training program found participants incorrectly failed candidates less and were more confident in their assessments.18,19 After an instructor program involving lectures, scenario development, and video reviewing, participants reported improved ability to conduct simulations, recognize warning signs, and debrief.12 In summary, evidence supports ongoing instructor development with targeted training programs and structured assessment techniques that improve instructor confidence, error detection, and teaching abilities.
| COR | LOE | Recommendations |
|---|---|---|
| 2b | C-LD | 1. The usefulness of alternative objects to train laypeople in chest compressions, when compared to a manikin, is not well established. |
Synopsis
Barriers to CPR training in low-resource settings include cost, access to training centers, and time constraints. Preliminary data about the feasibility of the use of common household objects to train and practice chest compressions have been recently described.1-6 The goal of these studies is to find low-cost, easy-access alternatives to manikins to allow laypeople in low resource settings to receive chest compression training at home without attending training courses.1-4,6-8 The underlying assumption is that such training is preferable to having no psychomotor training.
Recommendation-Specific Supportive Text
- Seven studies were identified where learners used alternative objects (eg, pillow, toilet paper rolls, foam blocks) to practice chest compressions.1-4,6-8 Four RCTs compared use of these objects to a standard manikin and assessed chest compression performance after training using a feedback-enabled manikin.2,3,6,8 Results were mixed, with 2 RCTs finding no difference in compression rate or depth2,3 and 2 finding worse compression depth with the alternative objects.6,8 One study found better chest wall recoil during manikin-based post training assessment in learners who trained on a pillow compared with a manikin.2 Two observational studies found favorable responses after training using these objects to surveys of usefulness and confidence.1,4
| COR | LOE | Recommendations |
|---|---|---|
| 1 | B-NR | 1. It is recommended that lay rescuers receive education on recognition and initial treatment steps for persons experiencing opioid-associated out-of-hospital cardiac arrest (OHCA). |
| 2b | C-LD | 2. The optimal training method for lay rescuers in recognizing and intervening on opioid overdose has not been established. |
Synopsis
According to the Centers for Disease Control and Prevention, opioid overdose deaths in the United States have more than doubled in the past decade, from 18 515 in 2007 to 47 600 in 2017.1 Improving recognition of opioid-associated OHCA and increasing lay rescuers’ willingness and ability to administer naloxone has the potential to improve outcomes.22 Systematic and scoping reviews on education for lay rescuers to recognize and intervene in opioid-associated OHCA have generally shown that training can increase knowledge and confidence, including a review specific to virtual instructional interventions.3-5 For the present review, studies comparing at least 2 instructional methods are included. There is a high degree of variability in study design, intervention, and outcome measures used, and several studies use self-reported outcome measures that may be particularly subject to bias.6-8 More research is required to determine which educational interventions provide the greatest benefit by measuring both learner and patient outcomes.
Recommendation-Specific Supportive Text
- Three recent systematic reviews summarized the impact of lay rescuer training in opioid overdose recognition and treatment.3-5 A systematic review of 87 studies found that lay rescuer training led to improved knowledge, improved willingness to respond, and increased likelihood of naloxone use3 A scoping review of 59 studies reported a correlation between naloxone distribution and survival, but acknowledged the heterogeneity in studies and difficulty summarizing specific recommendations for training.4 A scoping review of virtual training methods for lay rescuers found that such programs appear effective in increasing knowledge, confidence, and preparedness to respond.5
- Eight studies compared the impact of opioid training using 2 instructional methods. Comparisons included training with and without providing nalaxone,6,8 computer- or video-based training versus instructional sheet,7,9,10 different duration of training session,11 inclusion of a peer support intervention12 and a novel local program versus standard training.9 Outcomes were also heterogenous and included knowledge assessments,6,7,9,11,12 surveys of confidence,6 performance assessment in a simulated opioid overdose,9 and proportion of subjects who filled a prescription for naloxone.10
| COR | LOE | Recommendations |
|---|---|---|
| 1 | B-NR | 1. It is recommended to focus and tailor layperson CPR training to specific racial and ethnic populations as well as neighborhoods and to incorporate awareness efforts in these areas. |
| 1 | B-NR | 2. It is recommended to focus on low SES populations and neighborhoods for layperson CPR training and awareness efforts. |
| 1 | B-NR | 3. It is recommended to address barriers in performing layperson CPR on females through educational training and public awareness efforts. |
| 2a | C-LD | 4. It is reasonable to address barriers to linguistically isolated communities by increasing availability and access to CPR training materials in diverse languages. |
| 2a | C-LD | 5. It is reasonable to consider cost-effective methods for CPR training and to promote safe access to CPR training for low SES populations and neighborhoods. |
Synopsis
Health disparities adversely affect groups who systematically experience greater obstacles to health based on race, ethnicity, gender identity, geography, and SES. Historically, race, ethnicity, SES, sex, and gender are associated with different rates of layperson CPR.1-17 People experiencing cardiac arrest in racial and ethnic populations who have historically experienced inequity or prejudice, such as Black and Hispanic/Latino persons, and linguistically isolated communities with limited English proficiency have had lower rates of layperson CPR.18-23 Focusing and tailoring CPR training for these populations is needed, as well as those that consider cost-effectiveness and safe access to training in low SES settings.
Recommendation-Specific Supportive Text
- Retrospective cohort studies and 1 cross-sectional study found that residents of Black and Hispanic/Latino neighborhoods were less likely to receive CPR and that Black persons were less likely to be CPR trained.1,3-6,24,25 To address this, retrospective studies have demonstrated the feasibility of using neighborhood mapping to identify racial and ethnic neighborhoods for focused training.13,26
- Several retrospective cohort studies and 2 systematic reviews have demonstrated that low SES is associated with a lower likelihood of receiving LR-CPR.7-16,27 In addition, recent cross-sectional studies and 2 systematic reviews found that low SES is associated with a lower likelihood of CPR training.1,28-32 Additionally, individuals from low SES communities are less likely to report comfort performing CPR.33-35 To address this, retrospective studies have demonstrated the feasibility of using neighborhood mapping to identify low SES neighborhoods for focused training.13,26
- Studies examining sex differences in delivery of CPR found that adult females were less likely than males to receive LR-CPR in public locations.2,17,36 Cross-sectional survey studies suggest that layperson responders are fearful of being accused of inappropriate touching, sexual assault, and causing injury to females in need of LR-CPR.37,38 A randomized simulation study found that subjects were less likely to remove the clothing of a female manikin than a male manikin.39 The gender of the lay rescuer may impact receipt of CPR.40 Female respondents were less comfortable performing CPR than males.33,34,41
- A descriptive investigation found few high-quality CPR educational resources for Spanish-speaking populations.19 Mixed qualitative studies suggest that language barriers, financial considerations, and lack of information are associated with low rates of LR-CPR in linguistically isolated communities.18-23
- Financial costs of training, lack of information, and fear of risking one’s own life or safety are common barriers to CPR training in low SES neighborhoods.13,18,21,22,42
| COR | LOE | Recommendations |
|---|---|---|
| 1 | B-NR | 1. It is recommended to train middle school- and high school-age children to perform high-quality CPR. |
| 1 | C-LD | 2. It is recommended to start CPR training under 12 years of age in order to increase willingness and self-confidence in later years. |
Synopsis
Immediate CPR can double or triple survival rates after cardiac arrest.1,2 The primary goal of resuscitation training for lay rescuers (ie, non–health care professionals) is to increase immediate layperson CPR rates, AED use, and timely emergency response system activation during an OHCA. Enhancing willingness of children to perform CPR may have a direct impact on survival rates for OHCA by improving socialization of the need for CPR early.3,4 For this recommendation, schoolchildren are considered those who attend middle and high school, approximately 12 to 18 years of age.
Effective chest compression depths and ventilation volumes can be achieved on training manikins by 10 to 12 years of age. However, starting to introduce the concepts of emergency calls and the need for CPR and AEDs earlier in younger children improves socialization of the importance of timely lay rescuer response. Annual repetition of messaging and training in all children may increase willingness and self-confidence in later years. Schoolchildren also serve as multipliers by passing on BLS skills to others.5
Recommendation-Specific Supportive Text
- Multiple studies have found that middle school- and high school-age children are capable of learning, recalling and performing high-quality CPR skills.4-21 Evidence suggests that schoolchildren can only achieve effective resuscitation attempts with sufficiently deep and rapid chest compressions or adequate ventilation volumes at age 12 years of age or older.22-26
- Schoolchildren from 4 to 7 years of age can make an emergency call27-30 or follow the instructions of an automatic external defibrillator.27-29,31 In schoolchildren under 12 years of age, a playful approach in terms of CPR at early ages promotes motivation and interest.27-29,31-33 Annual repetition leads to a consolidation of practical CPR skills, which sustainably increases the willingness and self-confidence in initiating resuscitation measures in later years.28
| COR | LOE | Recommendations |
|---|---|---|
| 2a | C-LD | 1. It is reasonable to increase lay rescuer willingness to perform CPR through CPR training, mass CPR training, CPR awareness initiatives, promotion of Hands-Only (compression-only) CPR, and mobile apps alerting lay rescuers to emergency events. |
| 2b | C-LD | 2. It may be reasonable for lay rescuer CPR training programs to raise awareness of physical barriers that may affect lay rescuers’ willingness to perform CPR. |
| 2b | C-LD | 3. It may be reasonable for lay rescuer CPR training programs to address emotional barriers that may impact lay rescuers’ willingness to perform CPR. |
Synopsis
Prompt lay rescuer CPR (LR-CPR) delivery doubles survival for persons experiencing sudden cardiac arrest, yet fewer than 40% of these individuals receive LR-CPR.1,2 Given the relatively low LR-CPR rate, facilitator and performance barrier assessment of LR-CPR is warranted. Individual-level facilitators that increase willingness to perform LR-CPR include previous CPR training, younger age, and family relationship to the person experiencing cardiac arrest.3-6 Community-level facilitators include Hands-Only CPR training, mass CPR training (ie, training large numbers), CPR awareness initiatives to increase lay rescuer performance, and mobile apps to alert lay responders to emergency events.4,7-11 Barriers to lay rescuers initiating CPR include individual-level emotional barriers such as perception of the person’s physical characteristics (eg, vomit, blood), perceived futility of the situation, and difficulty or limitations with positioning of the patient.3,8,12-15
Recommendation-Specific Supportive Text
- A cohort study demonstrated that lay rescuers with previous CPR training were 3 times more likely to perform CPR.4 A 40-minute mass, Hands-Only CPR training of more than 5500 university students was found to promote LR-CPR.8 Community-level promotion of Hands-Only CPR training was associated with increased LR-CPR and an increased incidence of survival with favorable neurological outcome.7 Communities with a higher proportion of residents identifying as having CPR awareness, prior CPR training, and higher self-efficacy were associated with an increased likelihood of LR-CPR.9 Two studies of previously enlisted community first responders using a cellphone app which alerted them to emergencies found that responders to OHCA were facilitated to assist with LR-CPR with the information from the app (eg, location).10,11 Some studies were limited by prior CPR training and ecological community-level measurements.
- Several survey-based studies of lay rescuers described vomit, alcohol on the person’s breath, and visible blood as physical barriers to initiating CPR.12,15 Analyses of telecommunicator-assisted CPR tapes found that inability to move patients to a hard, flat surface was associated with reduced rates of CPR.13,14
- Observational studies found that panic, lack of confidence, perceptions of futility, and fear of injury were emotional barriers to initiating CPR.3,12 A survey of lay responders using a mobile app for emergency alerts cited logistical obstacles (eg, smartphone difficulties) and cognitive-emotional obstacles as barriers to accepting dispatch alerts.11 A survey of university students cited burden of responsibility and difficulty in judging a cardiac arrest as additional barriers.8 These studies suggest that tailored CPR training to address these emotional barriers and providing general awareness of these barriers may improve lay rescuer willingness to perform CPR.
| COR | LOE | Recommendations |
|---|---|---|
| 2a | C-LD | 1. It is reasonable for health care professionals to take an adult ACLS course or equivalent training.1-9 |
Synopsis
Resuscitation councils have offered adult ALS courses (eg, ACLS offered by the AHA, Advanced Life Support offered by the European Resuscitation Council) for more than 3 decades, providing the knowledge and skills required to recognize and treat critically ill adult patients.10 These courses are intended for health care professionals likely to manage adult patients with cardiac arrest. Advanced cardiovascular life support course content and instructional design is updated to reflect the most current resuscitation guidelines, and recent versions have focused on interprofessional, team-based care via simulation-based training.10-12
Recommendation-Specific Supportive Text
- A systematic review found evidence from 6 observational studies3-8 enrolling 1461 patients with higher rates of return of spontaneous circulation (ROSC) for adult in-hospital cardiac arrest cared for by a resuscitation team with at least 1 member completing an accredited ACLS course compared with patients cared for by a team without members with prior ACLS training.9 The systematic review found evidence from 7 observational studies1-3,5-8 enrolling 1507 adult in-hospital cardiac arrest patients for improved survival to hospital discharge or survival to 30 days for patients cared for by a team with at least 1 member completing an accredited ACLS course.9 Pooled data from 2 observational studies5,6 enrolling 455 patients showed no significant association between 1-year survival and ACLS training.9 Additional benefits of ACLS training include faster time to ROSC,5 decreased treatment errors (eg, incorrect rhythm assessment),4 and an association between the number of team members trained and ROSC.5 No studies report the impact of ACLS training on intact neurological survival or the impact of course components on patient outcomes. Among the studies reviewed, there was a high risk of selection bias due to differences between study populations. Most studies were conducted before 2010 and may not accurately reflect current standards of care and current ACLS course design, which has a greater focus on team-based care and simulation-based learning.
| COR | LOE | Recommendations |
|---|---|---|
| 2a | C-LD | 1. It is reasonable for EMS systems to monitor clinical personnel’s exposure to resuscitation events to ensure treating teams have members competent in the management of cardiac arrest cases. |
Synopsis
Appropriate provision of prehospital resuscitative care is an important element in determining outcomes from OHCA.13 Understanding the impact of ongoing exposure (ie, caring for actual patients in cardiac arrest) or general experience (ie, time on the job) on patient outcomes from OHCA may inform staffing and training strategies. A systematic review suggests that EMS professional exposure—both the number of cardiac arrest cases managed over time and the most recent exposure to cardiac arrest (less than 6 months)—is associated with improved ROSC14,15 and survival to hospital discharge.16,17 Results of the individual studies were inconsistent, but those of higher quality that adjusted for known predictors of survival demonstrated improved short-term survival outcomes with higher EMS professional exposure.16 Emergency medical service professional experience was not associated with improved survival to discharge.16
Recommendation-Specific Supportive Text
- Results of a systematic review identified 2 observational studies that evaluated an impact of professional exposure.15,16 The larger study reporting adjusted outcomes found improved survival to discharge with higher team exposure (number of cardiac arrests in the preceding 3 years). Compared with teams with fewer than 6 exposures, the likelihood of survival was higher in groups with more than 6 to 11 exposures, 11 to 17 exposures, and greater than 17 exposures, suggesting a dose-response relationship with exposure.16 The remaining observational study reporting unadjusted outcomes found no association between exposure and survival to hospital discharge. One observational study found lower survival to discharge in patients treated by teams with no exposure in the preceding 6 months compared with those with recent (less than 1 month) exposure.16 Additional studies found no association between team leader cardiac arrest exposure and event survival15 and no association between years of clinical experience of the EMS professional or EMS team and survival to hospital discharge.16,18,19 Two studies reported improved ROSC with higher prior exposure to resuscitation events in the primary treating paramedic.14,15
Knowledge Gaps and Future Research
Conducting impactful research on resuscitation education carries its own set of challenges, some of which are very different from the challenges of clinical research. The Grading of Recommendations Assessment, Development, and Evaluation system for evidence review, used throughout these Guidelines, has massive shortcomings in its applicability to educational research.1 The certainty assessment of evidence in Grading of Recommendations Assessment, Development, and Evaluation terms is reduced in the presence of risk of bias, imprecision, and indirectness. When one considers that blinding of assessors and participants in simulation studies is often impossible, that the majority of these studies are small and conducted with specific learner groups, and that virtually all of the studies reviewed for Part 12 were not associated with clinical outcomes, it is easy to see how rare it is for the certainty of the evidence to be any higher than moderate, and much more commonly low or very low. Larger, more generalizable studies featuring multicenter collaboration would help to address this problem. Education research networks provide the infrastructure necessary to support mentorship, grant applications, study design and implementation, and provide knowledge dissemination.2 Similarly, outcome measures that are reliable, reproducible, and clinically relevant are a goal to work toward with education research. When the selection of patient outcomes is not feasible, we encourage educational researchers to select quantitative measures that have a known association with improved clinical outcomes from cardiac arrest (eg, chest compression depth). Doing so will allow researchers to establish causal links among outcomes that are similarly reported in simulation-based and clinical studies.3
Very few of the recommendations in Part 12 are based on robustly conducted meta-analyses, and the ones that are (eg, feedback devices, manikin fidelity) exhibit very large degrees of heterogeneity. This too should not be surprising, given that these studies may involve many different learner groups (eg, students, nurses, physicians, paramedics, laypersons) and surrogate outcomes that can be measured and/ reported in a variety of ways (eg, overall chest compression quality, specific compression parameters such as depth and rate, timing considerations, etc.). The establishment of standardized reporting guidelines for outcomes from resuscitation education research would address this issue and enable meta-analysis of key questions in the future. Because very few studies link educational interventions to patient outcomes, additional research is needed to examine the connections between educational outcomes and survival from cardiac arrest, as well as from other intermediate clinical outcomes known to be contributors to survival, such as high-quality CPR. The growth and evolution of technology and its incorporation into educational design has implications that these Guidelines do not fully address. Perhaps most notably, well-conducted research evaluating the cost-effectiveness of the various technology-dependent elements of instructional design (eg, high-fidelity manikins, VR, AR, gamified learning, and cognitive aids on digital platforms, etc) is lacking in current literature. In addition to cost, implementing technologies such as these also requires personnel with appropriate training to use and maintain such devices. Training centers also require significant infrastructure such as physical space, basic equipment, and information technology support. The balance between cost and benefit will vary among institutions, regions, and nations. For example, a recent systematic review examining the effect of higher physical realism in training manikins for learners in low-resource settings failed to demonstrate any difference in skill or knowledge acquisition when compared with lower-realism devices; the authors of this review made a recommendation against the use of manikins with higher realism, presuming that the cost would outweigh the benefit.4 Future research should include elucidating the cost-benefit ratio of these evolving technologies. At the same time, we recognize the importance of incorporating digital and technologic advances to improve training quality and accessibility. We believe this will be an area where recommendations for resuscitation education may change most rapidly. In the section of Part 12 summarizing published data on VR, the writing group assigned a COR 3 (possible harm) for the use of VR for CPR skill training. This recommendation is based on the best available evidence, but we believe its implication may be different than for that of a COR 3 in another section of these Guidelines. For example, if a clinical intervention were found to have a negative association with patient outcomes from cardiac arrest and a COR 3 recommendation was assigned to it, it is easy to imagine that such an intervention would be abandoned from common clinical use. For an educational intervention—particularly one dependent on rapidly evolving technology—this is not necessarily the case, and with continual progress in VR and other technologies, we expect that ongoing reassessment of this literature will remain necessary, and that such recommendations may change over time. We continue to encourage the exploration and optimization of technology for resuscitation training.
Table 2 contains an exemplar list of knowledge gaps in resuscitation education from the various areas covered in Part 12. This list is far from complete but is meant to provide more focused ideas than the overarching concerns with education research discussed earlier. We are encouraged that Part 12, compared with that from the 2020 Guidelines,5 has a greater number of topics and many new recommendations, as well as some existing recommendations, yielding enough good-quality evidence to be strengthened to higher COR levels. We call on researchers to continue this progress toward higher-quality evidence for educational outcomes and to continue to strive for the elusive link to patient outcomes. Accordingly, we also urge research funding agencies to provide support to these critical endeavors. We call on educators to continue to interrogate the optimal means of implementation and dissemination of existing knowledge while determining the economic impact of recommended approaches. A multifaceted approach will be essential in strengthening this element of the formula for survival and thus improving outcomes from cardiac arrest.
|
Topic area |
Sample research topics |
|
General underexplored areas of research in resuscitation education |
Synergy between combinations of instructional design phenomena Educational impact over longer time periods Cost-effectiveness Consistency and generalizability of study outcomes Link to patient clinical outcomes |
|
Feedback devices in training |
Further studies exploring effects of training with feedback devices on CPR skill retention and transfer of CPR skills to the real clinical environment (eg, CPR quality during cardiac arrest events) to clarify the clinical effectiveness |
|
Rapid-cycle deliberate practice |
Consistent definitions of passing standard (eg, mastery) during RCDP-based training |
|
Spaced learning |
Optimal training frequency for specific provider groups, including selected lay rescuer populations (eg, coaches, lifeguards) and health care professionals |
|
Team training |
Evidence regarding the most efficacious training methods to improve teamwork competencies Guidance regarding the outcome measurement of teamwork competencies Evidence regarding which teamwork competencies have the greatest impact on technical skill performance and overall resuscitation performance in simulated and real cardiac arrests Evidence linking teamwork performance to clinical outcomes and patient safety |
|
Manikin fidelity |
Identifying simulation features most associated with learner engagement |
|
Gamified learning |
Consistent definition of gamification Impact of gamification on cognitive load and stress levels |
|
Virtual and augmented reality |
How AR and VR are best employed (eg, real-time feedback, gamification, knowledge delivery) Clarification of the instructor role with immersive technology is being used (eg, when is it beneficial for the instructor to provide feedback, and what type of training is needed when this technology is used?) |
|
Blended learning |
Defining the combination/sequence/timing of blended content delivery methods to yield the best outcomes |
|
Scripted debriefing |
Assessing the impact of scripted debriefing on knowledge and skill retention Defining the importance of debriefer adherence to debriefing scripts and its influence on learning and performance outcomes Assessing debriefer experience and learner characteristics on the impact of debriefing scripts |
|
Disparities in CPR education |
Evidence-based initiatives to focus and tailor layperson CPR training to underrepresented racial, ethnic, and low SES populations and neighborhoods Methods to remove barriers to performing CPR on female persons Enhanced diversity and culturally competent CPR training, including diversity in manikin design and appearance |
|
Willingness for lay rescuers to provide lay rescuer CPR |
Assessing effectiveness of public awareness interventions on CPR training participation willingness to perform CPR Identifying simple adjuncts (eg, pocket masks, hand/eye protection) and strategies for their dissemination to improve willingness to perform CPR |
|
CPR training for schoolchildren |
School-based training frequency to optimize educational outcomes |
|
Cognitive aids |
Comparison of method (eg, card versus smartphone versus mnemonic use) for cognitive aid Measurement of stress and/or cognitive load in learners and determine the impact of aids on these outcomes Effective design and dissemination of cognitive aids for lay rescuers |
AR indicates augmented reality; CPR, cardiopulmonary resuscitation; RCDP, rapid-cycle deliberate practice; and VR, virtual reality.
The American Heart Association requests that this document be cited as follows: Donoghue AJ, Auerbach M, Banerjee A, Blewer AL, Cheng A, Kadlec KD, Lin Y, Diederich E, Sawyer T, Stallings DT, Toft LEB, Wright JI, Schexnayder SM, Dainty KN. Part 12: resuscitation education science: 2025 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2025;152(suppl 2):S719–S750. doi: 10.1161/CIR.0000000000001374
- Aaron J. Donoghue, MD, MSCE, Chair
- Marc Auerbach, MD, MSc
- Arna Banerjee, MD, MMHC
- Audrey L. Blewer, PhD, MPH
- Adam Cheng, MD
- Kelly D. Kadlec, MD, Med
- Yiqun Lin, MD, MHSc, PhD
- Emily Diederich, MD
- Taylor Sawyer, DO, MBA, MEd
- Devita T. Stallings, PhD, RN, FAAN
- Lorrel E.B. Toft, MD
- Deborah Torman, EdD
- Jaylen I. Wright, PhD
- Stephen M. Schexnayder, MD
- Katie N. Dainty, PhD, Vice Chair
Open table in a new window.
Open table in a new window.
 Login
Login