Part 1: Executive Summary
Abstract
This executive summary provides an overview of the 2025 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care, which is organized around the Utstein Formula for Survival and provides updated recommendations aimed at improving survival rates and neurological outcomes following cardiac arrest. This executive summary outlines key changes, emphasizing the importance of high-quality chest compressions, early defibrillation, and the integration of advanced resuscitation techniques. These Guidelines also highlight critical post–cardiac arrest care strategies, including targeted temperature management and hemodynamic stabilization. Additionally, they stress the need for population-specific resuscitation approaches, particularly for pediatric patients, pregnant individuals, and individuals with cardiac arrest due to special circumstances. A strong focus is placed on continuous training and education for both medical professionals and lay rescuers to enhance the implementation and effectiveness of these lifesaving interventions. The 2025 Guidelines also highlight the importance of an integrated system of people, protocols, policies, and resources to achieve quality improvement in cardiac arrest care. An overview of ethical considerations relevant to emergency cardiovascular care, resuscitation, and approaches to decision-making surrounding cardiac arrest is also included. By following these updated recommendations, the American Heart Association seeks to optimize resuscitation efforts and improve patient outcomes in cardiac emergencies.
Introduction
The 2025 American Heart Association (AHA) Guidelines for Cardiopulmonary Resuscitation (CPR) and Emergency Cardiovascular Care (ECC) provide a comprehensive review of evidence-based recommendations for resuscitation and ECC. The Guidelines for CPR were first published in 1966 in response to requests from several organizations and agencies about the need for standards and guidelines regarding training and response..1
Since then, the CPR Guidelines have been reviewed, updated, and published periodically by the AHA.2–10 As with prior Guidelines, this document is closely aligned with evidence evaluation conducted by the 2025 International Liaison Committee on Resuscitation (ILCOR) and associated member councils. ILCOR was formed in 1992 to provide a forum for liaison between principal resuscitation organizations worldwide. At the time of this publication, ILCOR comprises representatives of 9 member organizations.11 Although the AHA generally publishes its Guidelines on a 5-year cycle, since ILCOR transitioned to a continuous evidence-evaluation process in 2015, the AHA has published focused updates between formal Guidelines when there is a substantial need for updated treatment recommendations based on new scientific evidence. This allows for expedited review and incorporation of significant changes in science directly into the Guidelines if deemed appropriate, increasing the potential for more timely transitions from guidelines to bedside. Since the publication of the 2020 Guidelines, there has been a significant expansion in the number of writing groups and chapters, including the addition of new chapters on post–cardiac arrest care, special circumstances, and ethics. The AHA ECC Committee has also strengthened partnerships with other organizations, such as collaborating with the American Academy of Pediatrics (AAP) to jointly publish and cochair the writing groups for pediatric basic life support (PBLS), pediatric advanced life support (PALS), and Nneonatal Resuscitation. Efforts have also been made to enhance synergy and streamline content across chapters and disciplines, ensuring consistency in overlapping topics, concepts (eg, a single Chain of Survival), terminology (eg, breaths, rescue breaths, ventilations), and algorithms. The chapter writing group members updated evidence reviews specific to the scientific questions considered of greatest clinical significance, with a focus on topics with new evidence.
Epidemiology and Outcomes
In the half century since the initial Guidelines were published, cardiac arrest remains a leading cause of mortality and morbidity in the United States and worldwide, making this work still incredibly relevant. Despite advances in treatment, incidence of cardiac arrest remains high, and survival remains low. We recognize and acknowledge the negative impact of COVID-19 on resuscitation survival outcomes and on health care and lay rescuer response to cardiac arrest. Epidemiologic trends since 2023 demonstrate a modest upward trend in out-of-hospital cardiac arrest (OHCA) survival rates.12 Recognizing the continued threat of infectious disease transmission, these 2025 Guidelines also include recommendations to reduce the risk of transmission of high-consequence respiratory pathogens during treatment of cardiac arrest (refer to Part 10: Adult and Pediatric Special Circumstances of Resuscitation).13
OHCA
As reported in the 2024 Cardiac Arrest Registry to Enhance Survival (CARES) Annual Report, the incidence of emergency medical services (EMS)–treated, OHCA in people of any age in the United States was 378.7 individuals per 100 000 population, with great variation in incidence and survival between states.12 There were an estimated 263 711 EMS-treated, nontraumatic OHCA cases in the United States in 2024. Survival to hospital discharge after EMS-treated adult OHCA was 10.5%, and favorable neurologic survival was 8.2%. Bystander-witnessed adult arrests where bystander CPR was initiated had a 13.0% survival to hospital discharge compared with the 7.6% survival to discharge for unwitnessed arrests (P<0.0001); however, only 41.7% of OHCA adult patients received bystander CPR. Survival to hospital admission after EMS-treated nontraumatic OHCA was 25.7% for all presentations. Survival to hospital discharge was higher when the cardiac arrest occurred in a public place (21.1%) than if it occurred in a residential setting (8.9%) (P<.0001). Only 12.6% of patients who experienced cardiac arrest in public had an automated external defibrillator (AED) applied by a lay rescuer. As reported in the “2025 Heart Disease and Stroke Statistics: A Report of US and Global Data from the American Heart Association,”14 83% of the EMS-treated OHCAs in children were in private residences while 16.7% were in public places. Survival to hospital discharge was 7.4% for 1587 children < 1 year of age, 14.1% for 1225 children 1 to 12 years of age, and 18.5% for 854 children 13 to 18 years of age.
In-Hospital Cardiac Arrest
Incidence of in-hospital cardiac arrest (IHCA) in adults each year in the United States is estimated to be about 292 000 patients as extrapolated using the AHA’s Get With The Guidelines Resuscitation data.14 According to the 2023 data used in this report, survival to hospital discharge was 23.6% for adult patients with IHCA and among survivors, 79.2% had favorable neurologic outcome (Cerebral Performance Category 1 or 2) at hospital discharge.12 Survival to hospital discharge after IHCA in pediatric patients (children and infants 0–18 years of age) increased from 18.9% to 45.2% between 2000 and 2023 in the Get With The Guidelines®-Resuscitation data.12 The notable increase in survival is multifactorial in nature, including early recognition of deterioration and the provision of high-quality CPR.
Disparities and Differences
Despite advances in resuscitation care, inequities in survival outcomes persist. In the 2025 AHA Statistics Update, it was noted that survival and neurological recovery after cardiac arrest were worse in minoritized racial and ethnic groups, including Hispanic, Black, and Asian individuals, compared with non-Hispanic White individuals. White people had a higher chance of a favorable neurologic outcome than those from minoritized groups (34.4% versus 21.7%, respectively; P=0.015).14 Individuals from racial and ethnic groups that have been historically marginalized are also more likely to have early severe electroencephalogram (EEG) or computerized tomography anoxic changes (25.0% versus 15.8%, respectively; P=0.03).14
The causes of these disparities are complex and are closely associated with socioeconomic disadvantage and unequal access to care. Unequal provision of CPR and use of an AED by lay rescuers contribute to worse cardiac arrest outcomes and are the result of unequal access to lay rescuer CPR and AED training opportunities.15 There is also increasing evidence of differences based on population density—eg, rural versus metropolitan—with the odds of OHCA survival to hospital discharge being approximately 50% lower in rural areas compared with metropolitan areas.16 Thus, the translation of guidelines and science into educational resuscitation training products must consider the needs of all patients in their development with additional emphasis on equitable delivery and accessibility, especially in low-resource settings. This topic is discussed further in “Part 12: Resuscitation Education Science” of the 2025 Guidelines. Furthermore, despite the existence of evidence-based treatment guidelines, implementation varies widely due to unequal resource availability and access to care. The AHA ECC 2030 Impact Goals have an explicit focus on health equity and ensuring that cardiac arrest survival and access to care are equitable for all.15 In alignment with the ECC 2030 Impact Goals, the 2025 Guidelines highlight areas of opportunity to save more lives by prioritizing equitable delivery of lifesaving interventions throughout the Chain of Survival and including equitable outcomes as a measure of success. Additional considerations related to equity are included in “Part 3: Ethics.”
Chain of Survival and Newborn Chain of Care
Much of the variation in survival rates is thought to be due to differences across the Chain of Survival (Figure 1), the critical actions that must occur in timely succession to maximize survival from cardiac arrest.18 A sixth link in the Chain of Survival was introduced in the 2020 Guidelines, with different versions for adult, pediatric, IHCA, and OHCA.19 The 4 chains introduced in 2020 have now been consolidated to a single 6-link chain of survival for the 2025 Guidelines. Missing from this chain is the topic of prevention, which the writing group considered important but would like to better define before adding a seventh link.
Similarly, successful neonatal resuscitation depends on a continuum of integrated lifesaving steps that begins with careful assessment and preparation in advance of birth as well as resuscitation and stabilization at the time of birth and through the first 28 days after birth. The 2025 Guidelines introduce the Newborn Chain of Care (Figure 2), which addresses the broader context in which neonatal resuscitation occurs. With the recognition that the care and, therefore, the outcomes of parents and newborns are inextricably linked, the 7-link newborn chain of care differs from the Chain of Survival in that it starts with how health systems provide prenatal and intrapartum care (prevention), extending to postpartum, postresuscitation, and follow-up care that can optimize outcomes for parents and their newborns.
Terminology
Standardized terminology helps improve communication and accuracy in emergency response education. The 2025 Guidelines clarify the distinction between breaths and ventilations to ensure consistency in training and guidelines. To simplify nomenclature, the term rescue breaths is no longer used. Instead, breaths should be used when a person has a pulse but is not breathing and when breaths are given in conjunction with CPR, as in CPR with breaths. Ventilations should be reserved for health care professionals when providing assisted breathing through a mechanical device, such as a bag-mask device or an advanced airway device.
Similarly, lay rescuer was selected as the preferred term over layperson or lay responder when discussing care provided by non–health care professionals. The term lay rescuer is favored over bystander as it encourages action. Bystander can imply someone who is merely present but not taking action. The term lay rescuer clarifies the role and encourages action, reinforcing the vital role that people without medical training can play in an emergency.
The 2025 Guidelines also recognize the differential use of the abbreviations ROSC (return of spontaneous circulation) versus ROC (return of circulation) in the literature. For the purposes of these Guidelines, when return of circulation after CPR is achieved by mechanical means (eg, extracorporeal membrane oxygenation), the term ROC is preferentially used. When return of spontaneous circulation is due to recovery of cardiac function without mechanical intervention, the term ROSC is used.
Utstein Formula for Survival
This executive summary provides an overview of and orientation to the 2025 Guidelines, which are organized around the Utstein Formula for Survival (Figure 3).20 The Utstein Formula emphasizes that survival depends on 3 interactive factors: guideline quality (science), efficient education of patient caregivers (education), and a well-functioning Chain of Survival at a local level (local implementation). Local implementation, in turn, is largely dependent on systems of care (SOC), which incorporate the links within the Chain of Survival. Each section in this summary describes the scope of each Part of the Guidelines, along with a list of the most significant and impactful new or updated recommendations for that Part. Each section also includes a list of critical knowledge gaps that highlight important research questions and significant opportunities for enhancing the Chain of Survival. This executive summary does not contain extensive external reference citations; refer to Parts 2 through 12 for more detailed reviews of the scientific evidence and corresponding recommendations.
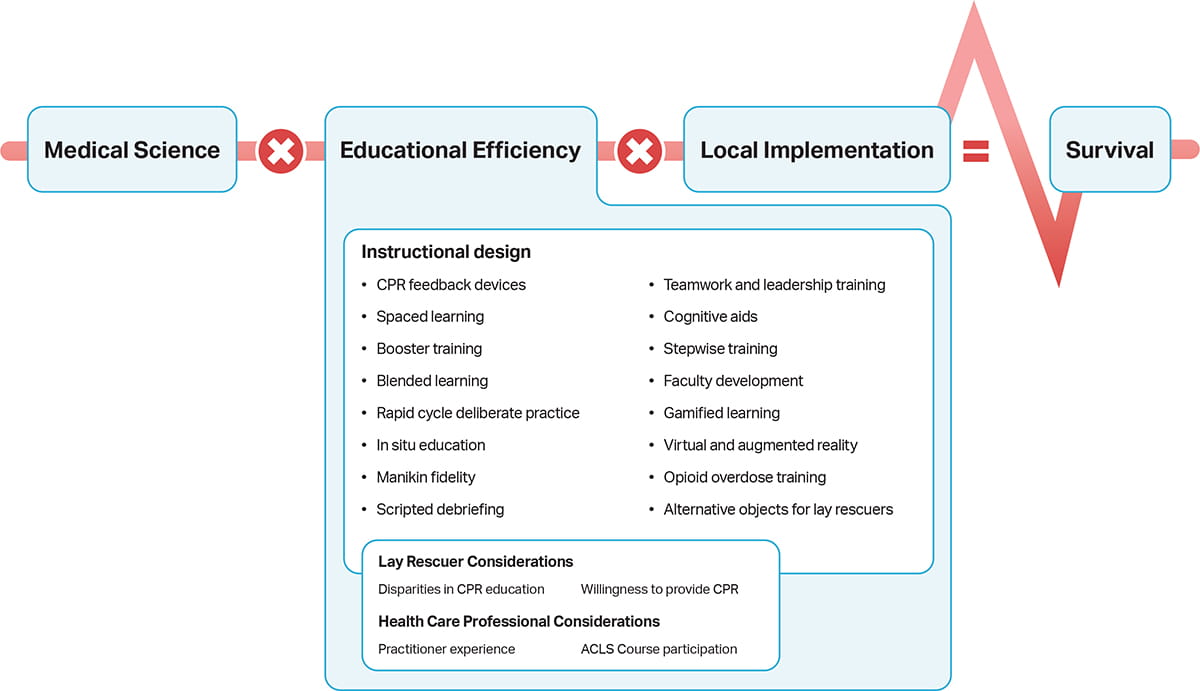
Figure 3. The Utstein Formula for Survival, emphasizing the 3 components essential to improving survival. 20
Reprinted from Soreide E, Morrison L, Hillman K, Monsieurs K, Sunde K, Zideman D, Eisenberg M, Sterz F, Nadkarni VM, Soar J, Nolan JP. Copyright 2013, with permission from Elsevier.
Introduction
The 2025 Guidelines are designed to present a comprehensive compilation of guidance for CPR and ECC.21 These guidelines are based on an evidence evaluation process conducted by ILCOR,22 published as systematic reviews, scoping reviews, and evidence updates published since the 2020 Guidelines as well as an independent evidence review process conducted by the 2025 Guideline Writing Groups. Together, these resulted in a description of the literature that facilitated guideline development.
Each chapter of the 2025 Guidelines is organized in knowledge chunks that are grouped into discrete modules of information on specific topics or management subjects. Each modular knowledge chunk includes a table of recommendations; a brief introduction or synopsis; recommendation-specific supportive text; hyperlinked references; and, when relevant, figures, flow diagrams or algorithms, and additional tables. Each chapter has undergone blinded peer review by subject matter experts and was also reviewed and approved for publication by the AHA Science Advisory and Coordinating Committee and the AHA Executive Committee. Chapters with pediatric content (neonatal resuscitation, pediatric basic and advanced life support) were also cochaired by the AAP and reviewed and approved by the AAP Board of Directors. The AAP also submitted names for peer review of the 2025 Guidelines and appointed one writing group member to each of the Evidence Evaluation, Ethics, Special Circumstances, and Systems of Care Writing Groups.
Each 2025 writing group reviewed all relevant and current AHA Guidelines for CPR and ECC,10,19,23–27 pertinent evidence evaluations and recommendations published in the International Liaison Committee on Resuscitation Consensus on Science With Treatment Recommendations since 2020, AHA Focused Updates,28–37 and all AHA evidence evaluation worksheets to determine if current guidelines should be reaffirmed, revised, or retired or if new recommendations were needed. The writing groups then drafted, reviewed, and approved recommendations after a thorough review of the literature for each topic, assigning to each a Class of Recommendation (COR; ie, strength) and Level of Evidence (LOE; ie, quality), as first described by Levine, et al. (2019)38 and outlined in Table 1 in “Part 2: Evidence Evaluation and Guidelines Development” of this supplement.21 Each knowledge chunk presents an overview of insights, including knowledge gaps and research priorities identified by writing group consensus discussions. A summary of knowledge gaps identified by the writing groups is included in this Executive Summary below. AHA policy requires that official positions and guidelines of the AHA must be reviewed and approved by the Board of Directors and/or its Executive Committee. Upon completion of peer review, these guidelines were reviewed and edited for publication by the AHA Science Advisory and Coordinating Committee and the AHA Executive Committee following the standard review process for all official AHA documents with legal, communications and science staff to ensure risk mitigation and accurate alignment with AHA mission.
The 2025 Guidelines contain 760 recommendations (Table). Despite recent improvements in support for resuscitation research, 38% of these recommendations are based on limited data. This highlights the persistent knowledge gaps in resuscitation science that need to be addressed through expanded research initiatives and funding opportunities.
Open table in a new window.
Ethics
“Part 3: Ethics” provides an overview of ethical considerations that are particularly relevant to ECC and resuscitation.39 This discussion is divided into 4 main sections. First, the chapter provides an overview of key frameworks in medical ethics that provide a structure through which health care professionals can analyze difficult decisions. In addition to principlism, which is organized around the principles of autonomy, justice, beneficence, and nonmaleficence and is currently the dominant medical ethical framework, the discussion highlights the importance of dignity and equity in ECC. Second, the authors summarize common approaches to ethical decision-making in ECC, including advanced directives, protocols, and shared decision-making. The chapter then discusses the specific decision to withhold or terminate CPR in adults and special populations, such as geriatric patients, children, and newborn infants. Additional consideration is given to the ethical complexity of prognostication and uncertainty, decisions to withhold or withdraw potentially ineffective therapies, and cultural and religious considerations. Finally, authors considered other selected ethical topics of importance in ECC. These include the process of research and knowledge generation (including guidelines development); the impact on health care professionals, patients, and families of providing, receiving, or witnessing resuscitation; crisis standards of care; advanced therapies, such as mechanical circulatory support; and organ and tissue donation. Ethics is most relevant to complex situations where there is not a single correct course of action and the process of knowledge generation differs from other medical domains. Thus, the chapter is presented in narrative format, rather than as modular chunks, and refrains from making evidence-based treatment recommendations.
Systems of Care
Survival after cardiac arrest requires an integrated system of people, protocols, policies, and resources along with ongoing data acquisition and review to achieve quality improvement. Such SOC, which are highly influenced by the environment in which they operate, produce efficiency and effectiveness in responding to cardiac arrest. Within the Utstein Formula for Survival (refer to Figure 3), SOC represents the operational means by which local implementation occurs. The objective of a cardiac arrest SOC is to quickly, efficiently, and effectively perform each step within the Chain of Survival.
Part 4 of the 2025 Guidelines, “Systems of Care,” focuses on elements that are relevant to a broad range of resuscitation situations.40 Previous SOC guidelines have identified a Chain of Survival (refer to Figure 1), beginning with prevention and preparedness to resuscitate and proceeding through resuscitation to post–cardiac arrest care, survivorship and recovery. The SOC guidelines include recommendations on training of specific personnel, implementation of protocols that have been demonstrated to be effective, and incorporation of nonhuman resources to optimize cardiac arrest care with ongoing debriefing and quality-improvement strategies. Germane to OHCA, this Part contains recommendations about EMS team composition and transport, community initiatives to promote lay rescuer response, public access to defibrillation and naloxone, and the role of emergency telecommunicators. Germane to IHCA are recommendations about cardiac arrest prevention and code team composition. Finally, this Part includes recommendations about extracorporeal membrane oxygenation CPR, cardiac arrest centers, organ donation, survivorship systems, and performance measurement across the continuum of resuscitation.
Significant New and Update Recommendations
Prevention of IHCA
We have combined the recommendations for adult and pediatric early warning systems and rapid response teams and recommend both as a means for preventing IHCA (early warning systems: COR 2a, LOE B-R; rapid response teams: COR 2a, LOE B-NR). The use of safety huddles is now recommended for patients identified as high risk to prevent IHCA (COR 2a, LOE B-NR).41-43
Public Access to Naloxone
Two new recommendations advise the implementation of public policies that permit the use of naloxone in cases of suspected opioid overdose without fear of prosecution (COR 1, LOE B-NR)44-46 and that support public distribution of naloxone through various means (COR 2a, LOE B-NR).47,48
Community Initiatives to Promote Lay Rescuer Response to OHCA
Prior recommendations on mobile technologies were combined into this knowledge chunk aimed at using various means to encourage lay rescuer CPR and use of AEDs. Recommendations are now provided on community education (COR 2a, LOE B-NR),49-52 mass media campaigns (COR 2b, LOE C-LD),53 policies supporting mandatory CPR certification (COR 2b, LOE C-LD),54,55 the use of mobile technologies (COR 2a, LOE B-NR),56-58 and bundled approaches (COR 2a, LOE B-NR) to achieve higher rates of lay rescuer response.59-62
Telecommunicator Recognition and Instructions
Recommendations regarding telecommunicator recognition of OHCA were strengthened (COR 1, LOE C-LD),63 and the LOE for providing compression-only instructions in adult OHCA was raised (COR 1, LOE A) in recognition of a meta-analysis of randomized trials that supports this recommendation.64
Team Composition for OHCA and IHCA
New recommendations are provided on the resuscitation team composition within the in- and out-of-hospital settings. These support the inclusion of at least one team member with advanced cardiac life support training (OHCA: COR 2a, LOE B-NR; IHCA: COR 1, LOE B-NR) and the delineation of roles with sufficient team size to achieve these roles (OHCA: COR 2a, LOE B-NR; IHCA: COR 2a, LOE B-NR).
On-Scene OHCA Resuscitation
New recommendations are made supporting ongoing resuscitation at the scene of OHCA in most cases, as opposed to early transport to a hospital (COR 2a, LOE B-NR).65-67 This strategy will necessitate termination of resuscitation on scene in many cases, and, therefore, it is recommended that EMS be trained in death notification to family and friends, which is a challenging task (COR 1, LOE B-NR).68-70
Cardiac Arrest Centers
In light of a recent randomized controlled trial (RCT) that did not support transport of post–cardiac arrest patients to regionalized centers of excellence,71 and acknowledging the lack of certainty about criteria that define a cardiac arrest center, the class of this recommendation was reduced from 2a to 2b and the LOE was increased to B-R (COR 2b, LOE B-R).
Extracorporeal Membrane Oxygenation CPR SOC
A new knowledge chunk pertaining to the components of an SOC intended to support extracorporeal CPR (ECPR) has been added. Four new recommendations provide guidance on the components of an SOC that are needed to support ECPR. These include recommendations regarding patient selection (COR 2a, LOE C-LD), cannulation strategies (COR 2a, LOE C-LD), regionalization of ECPR (COR 2a, LOE C-LD), and intra-arrest transport to regionalized ECPR centers (COR 2b, LOE B-R).
Organ Donation
Included is a new Class 1 recommendation (COR 1, LOE C-EO) that institutions develop SOC intended to evaluate patients who have had a cardiac arrest and who are unlikely to have a favorable outcome for the possibility of organ donation.
Survivorship and Rehabilitation Systems
We now recommend (COR 2a, LOE B-R) that institutions create SOC that span inpatient and outpatient domains to evaluate cardiac arrest survivors for disabilities and to provide them ongoing support to optimize recovery.72-77
Clinical Debriefing
We reiterated prior recommendations on clinical debriefing and added a new recommendation to consider incorporating immediate (hot) and delayed (cold) debriefing as a means to achieve system improvement (COR 2a; LOE C-EO).
Knowledge Gaps
Resuscitation science continues to evolve, with a growing understanding as new literature emerges of how integrated SOC impact clinical outcomes. Although many areas still require further study, the writing group felt that the following questions represent the most important knowledge gaps in SOC and, therefore, deserve the highest priority for future research:
- How can mobile technologies best be used to increase witness status in OHCA and resuscitation by lay rescuers to maximize opportunities for early intervention?
- What are the most cost-effective and feasible community interventions (including use of novel mobile technologies and drones) to optimize lay rescuer response to OHCA?
- Does telecommunicator-assisted conventional CPR (with breaths) offer improved outcomes compared with telecommunicator-assisted compression-only CPR in pediatric OHCA?
- Do specific etiologies of OHCA (eg, opioid-associated OHCA) warrant telecommunicators encouraging lay rescuers to perform conventional CPR (with breaths) over compression-only CPR?
- What are the patient characteristics wherein rapid response team and medical emergency team programs provide the greatest outcome benefits? Which interventions are most effective? Should automated early warning scores be linked to rapid response team or medical emergency team programs?
- What are the optimal timing, methods, and specific components of feedback or debriefing after attempted cardiac arrest resuscitation?
- How should behavior and leadership skill training be applied to code teams and EMS systems to optimize resuscitation?
- How can out-of-hospital and in-hospital datasets best be integrated as part of quality-improvement programs and research within SOC?
- Which patients warrant transport to a hospital with ongoing CPR, and what are the safest means of doing so while maintaining high-quality CPR?
- What constitutes a regionalized cardiac arrest center justifying longer transport times based on improved outcomes?
Neonatal Resuscitation
Part 5 of the 2025 Guidelines, “Neonatal Resuscitation,” includes recommendations on following the resuscitation algorithm through steps of anticipation and preparation, umbilical cord management at delivery, initial actions, temperature maintenance, heart rate monitoring, respiratory support, chest compressions, intravascular access and therapies, withholding and discontinuation of resuscitation, and postresuscitation care.78 These recommendations were developed by a multidisciplinary team of experts led by volunteer experts from the AHA and AAP. Consistent with the Utstein Formula for Survival (refer to Figure 3), the 2025 Guidelines provide a comprehensive review of recommendations for neonatal resuscitation, including new and updated recommendations that are based on the latest evidence from studies published in the medical literature and reviews completed by ILCOR.79 These recommendations are also inclusive of and have updated upon the 2023 update to the neonatal resuscitation guidelines.80
Significant New and Update Recommendations
Umbilical Cord Management
Deferring umbilical cord clamping in most instances for at least 60 seconds after birth can be beneficial in both term (COR 2a, LOE B-R) and preterm (COR 1, LOE A) newborn infants who do not require immediate resuscitation.37 For nonvigorous term newborn infants (and late preterm infants ≥ 35 weeks’ gestation), intact cord milking may be reasonable when compared with immediate cord clamping (COR 2b, LOE B-R) because it may reduce the need for cardiorespiratory support.81 Cord milking is not recommended for newborn infants <28 weeks’ gestation because it is associated with intraventricular hemorrhage (COR 3: Harm, LOE B-R).82
Oxygen
Oxygen concentration should be adjusted using pulse oximetry to target goals (COR 1, LOE C-EO). The initial oxygen concentration when providing ventilation is 21% for term and late preterm newborn infants ≥ 35 weeks’ gestation (COR 2b, LOE C-LD).83 For preterm newborn infants 32 to 35 weeks’ gestation, it may be reasonable to begin with 21% to 30% oxygen, with higher initial oxygen concentration for preterm infants < 32 weeks’ gestation (COR 2b, LOE C-LD), as a recent meta-analysis reported that high initial oxygen concentration may be associated with lower mortality.84, 85
Providing Assisted Ventilation
For term newborn infants, initial peak inflation pressures of up to 30 cm H2O are reasonable, with adjustment of peak inflation pressures as needed (COR 2a, LOE C-LD).86 For preterm newborns, initial peak inflation pressures of 20 to 25 cm H2O are reasonable, with adjustment of peak inflation pressures as needed (COR 2a, LOE C-LD).87
Ventilation Corrective Maneuvers
Ventilation corrective maneuvers can be useful when initial positive pressure inflations are not effective in newborn infants who require ventilation (COR 2a, LOE C-LD).88 Video laryngoscopy compared with traditional laryngoscopy can be useful for newborn infants who require endotracheal intubation (COR 2a, LOE B-R).79
Devices and Interfaces
A laryngeal mask, also referred to as a supraglottic airway, can be used as the primary interface to provide ventilation for newborn infants ≥ 34 weeks’ gestation (COR 2b, LOE C-LD).89 It can also be an alternative airway used in the process of corrective ventilation steps when face-mask ventilation is not effective ( COR 2a, LOE C-LD).90 A T-piece resuscitator can be beneficial to administer ventilation to newborn infants, particularly for preterm infants, because it may reduce the duration of ventilation and decrease the risk of bronchopulmonary dysplasia ( COR 2a, LOE B-R).91
Newborn Chain of Care
The Newborn Chain of Care addresses the broader context in which neonatal resuscitation occurs and how systems, starting from prenatal care and extending to postresuscitation and follow-up care, can optimize neonatal outcomes.
Knowledge Gaps
Some of the most pertinent gaps in neonatal resuscitation research include the following:
- What is the optimal initial oxygen concentration and oxygen titration strategy for preterm newborn infants requiring resuscitation?
- What is the optimal interval between birth and clamping the umbilical cord, and what interventions should be provided during this interval?
- Which term infants are best supported with continuous positive airway pressure versus supplemental oxygen or close observation without intervention?
- What are optimal adjustment strategies after starting assisted ventilation for positive end-expiratory pressure and peak inflation pressure?
- Can algorithms using large data sources predict which babies will require resuscitation or predict the likelihood of death or very poor neurodevelopmental outcome, and can corresponding tools impact clinical outcomes?
Pediatric Basic Life Support
Part 6 of the 2025 Guidelines, “Pediatric Basic Life Support,” includes recommendations for the treatment of pediatric OHCA and IHCA for patients outside of the newborn period.92 In contrast to the 2020 Guidelines, which combines PBLS and PALS in the same chapter (“Part 4: Pediatric Basic and Advanced Life Support”),25 this 2025 summary focuses solely on PBLS. These recommendations were developed by a multidisciplinary team of experts led by volunteer experts from the AHA and AAP. The causes, treatment, and outcomes of cardiac arrest in children differ from those of cardiac arrest in adults. For example, pediatric cardiac arrests are more often due to respiratory causes that progress to cardiac arrest rather than a primary cardiac event. These Guidelines contain recommendations for PBLS that are based on the best available resuscitation science. These apply to infants and children up to signs of puberty in the prearrest and intra-arrest phases of care in multiple settings, including the community, prehospital, and hospital environments. Topics reviewed include cardiac arrest in special circumstances, such as severe foreign body airway obstruction (FBAO). This summary highlights the new and updated recommendations in PBLS since 2020 that will have a significant impact on process- and patient-related outcomes from cardiac arrest. Additional recommendations related to pediatric resuscitation can be found in “Part 4: Systems of Care” and “Part 10: Adult and Pediatric Special Circumstances of Resuscitation.”
Significant New and Update Recommendations
Emphasis of Breaths With Chest Compressions
Despite increasing frequency of compression-only CPR in adults and children and mixed results when comparing conventional CPR (chest compressions and breaths) and compression-only CPR, large observational studies in children with OHCA show the best outcomes with conventional CPR.93-104 A small observational study of school-aged children found similar outcomes between conventional and compression-only CPR (COR 1, LOE B-NR).104 Large observational studies of children with OHCA do, however, show that compression-only CPR is superior to no lay rescuer CPR (COR 2a, LOE B-NR).
Elimination of 2-Finger Compression
In infants, systematic reviews and meta-analyses from simulation studies suggest that the 2 thumb–encircling hands technique is a superior technique when compared with 2-finger compressions, particularly for depth.105-109 In a multicenter, prospective observational registry study, the 1-hand technique resulted in greater compression depth than the 2-thumbs technique in infants, with no difference in chest compression rate between hand positions.110 The 2-finger technique was utilized rarely in this study but, when used, no chest compression segments were compliant with AHA pediatric guidelines (COR 1, LOE B-NR).110
Minimizing Perishock Pauses
Prolonged pauses in chest compressions before and after shock delivery decrease blood flow and oxygen delivery to vital organs, such as the brain and heart, and are associated with decreased survival (COR 1, LOE C-EO).111,112
Foreign Body Airway Obstruction
A recent observational study of adult FBAO suggests improved clearance of a foreign body with the use of back blows over abdominal thrusts.113 To create consistency for instructional purposes, and in the absence of inferiority from pediatric data, management of severe FBAO in children now starts with cycles that alternate 5 back blows, followed by a series of 5 abdominal thrusts, repeating as necessary (COR 1, LOE C-LD).
Knowledge Gaps
Some of the most pertinent gaps in pediatric resuscitation research include the following:
- What are the optimal chest compression metrics for pediatric resuscitation regarding compression depth, rate, and fraction (to include details about the timing and duration of pauses)? Do the optimal performance metrics change according to age or etiology?
- With what frequency should the rhythm and pulse be checked during CPR?
- What is the optimal ventilation rate during CPR in patients with or without an advanced airway? Is it age dependent?
- What is the optimal position for performing chest compressions (eg, on a step stool, kneeling on the bed, standing)?
- What is the effect of leaning on the chest and providing incomplete expansion of the chest in between chest compressions?
- What is the ideal concentration of oxygen to deliver when performing CPR?
- What is the ideal compression-to-ventilation ratio?
- What are the optimal timing and dosing of defibrillation for ventricular fibrillation (VF) and pulseless ventricular tachycardia (VT) and its interface with CPR?
- What clinical tools can be used to help in the decision to terminate pediatric IHCA or OHCA resuscitation?
- What is the effectiveness of a single shock compared with sequential (stacked) shocks in pediatrics?
- What is the adverse impact of shocking nonshockable rhythms with a manual defibrillator in IHCA?
- Is the time to shock with self-adhesive pads significantly different than with paddles?
- Is there an optimal pad position for defibrillation in pediatrics? If so, is it anteroposterior or anterolateral?
- Are there comparative pediatric population-based data for FBAO interventions (chest compressions versus abdominal thrusts)?
- What are the safety and efficacy of commercial devices to treat FBAO?
Adult Basic Life Support
Part 7 of the 2025 Guidelines, “Adult Basic Life Support,” provides recommendations for adults experiencing cardiac arrest, respiratory arrest, and FBAO.114 Early provision of high-quality CPR and prompt defibrillation are the key interventions to improve outcomes from adult cardiac arrest. The chapter addresses the recognition of cardiac arrest, the initial steps of CPR, and specific aspects of performance, such as rate and depth of chest compressions. Algorithms are provided to illustrate the sequence of resuscitation for adult cardiac arrest and interventions for FBAO. One notable change to the adult basic life support (BLS) algorithm is the inclusion of naloxone use by lay rescuers during respiratory and cardiac arrest. For purposes of these Guidelines, persons with signs of puberty are treated using the recommendations for adult BLS, while prepubertal children are treated using the recommendations in “Part 6: Pediatric Basic Life Support.”
Significant New and Update Recommendations
Foreign Body Airway Obstruction
Based on additional evidence of effectiveness and safety, the use of back blows is now recommended as the initial step for conscious adults with FBAO, followed by abdominal thrusts (COR 1, LOE B-NR).113 As in 2020, once the person becomes unresponsive, the recommendation is to initiate CPR (COR 1, LOE C-LD), with inspection of the mouth for presence of a foreign body prior to delivery of breaths (COR 1, LOE C-EO). A new algorithm for treatment of FBAO for adults is included.
Fundamentals of Ventilation
The use of breaths with chest compressions is recommended for both health care professionals (COR 2a, LOE C-LD) and lay rescuers (COR 2a, LOE B-R) when they are willing and capable. For lay rescuers who are willing to perform breaths, the use of a pocket mask, a face shield, or mouth-to-mouth breaths is acceptable. Providing breaths by using a pocket mask has been shown to deliver more effective breaths than using a face shield, so a pocket mask should be used if available. Observational studies suggest that breaths provided during CPR are often inadequate, so rescuers and health care professionals are advised to deliver each breath until there is visible chest rise (COR 2a, LOE C-LD).115
Positioning and Location for CPR
The effectiveness of chest compression delivery can be improved through optimizing rescuer hand position, rescuer body position, and patient position. Whenever possible, CPR should be performed on a firm surface. A rescuer should position themselves so that their knee is aligned with the patient’s torso, either by kneeling next to the patient or using a step stool for improved chest compression quality (COR 1, LOE B-NR). During the COVID-19 pandemic, the use of prone positioning for patients with hypoxic respiratory failure led to increased experience with the use of prone CPR. While the supine position is preferred, rescuers can consider providing CPR in the prone position if the supine position is not possible or would lead to significant delays in initiation of compressions (COR 2b, LOE C-LD).116
Feedback Devices and Mechanical CPR
Based on additional studies, the use of real-time feedback devices during CPR is recommended to improve manual CPR performance (COR 2a, LOE B-R).117 Studies comparing mechanical to manual CPR have shown that mechanical CPR is no better than manual CPR in improving patient survival. At present, the routine use of mechanical CPR devices is not recommended (COR 3-No Benefit, LOE B-R) but may be considered in specific circumstances in which high-quality CPR cannot be maintained or for health care professional safety, such as during transport to a hospital (COR 2b, LOE C-LD).
Knowledge Gaps
Questions that address some of the most pertinent gaps in adult resuscitation research include the following:
- What is the optimal sequence of interventions for adults with severe FBAO?
- What are the most reliable indicators to quickly and accurately identify cardiac arrest in adults?
- Should health care professionals check for a pulse prior to initiation of CPR?
- What is the optimal pad configuration (eg, anterior-lateral versus anterior-posterior) to improve defibrillation success?
- What is the optimal time interval for duration of chest compressions after shock delivery and prior to reassessing rhythm? Are there methods to assess presence of a perfusing rhythm prior to the current 2-minute interval?
- Are asynchronous breaths or ventilations effective during continuous chest compressions without an advanced airway?
- What is the optimal chest compression depth, rate, and duty cycle for adult cardiac arrest?
- What is the optimal chest compression fraction during CPR by trained lay rescuers and health care professionals?
- Are there noninvasive techniques for measuring blood flow during CPR that could guide performance of chest compressions?
- What are the appropriate targets for ventilation volumes and rates during BLS care of an adult patient who is in cardiac arrest?
- Can respiratory volume monitoring provide accurate measurements during CPR? What is the optimal ventilation rate and volume for an adult with absent or abnormal breathing but with presence of a pulse?
Pediatric Advanced Life Support
Part 8 of the 2025 Guidelines, “Pediatric Advanced Life Support,” includes recommendations for the treatment of pediatric OHCA and IHCA, including post arrest care and survivorship.118 These Guidelines contain recommendations for PALS and are based on the best available resuscitation science. These recommendations were developed by a multidisciplinary team of experts led by volunteer experts from the AHA and AAP. For the purposes of the PALS guidelines, pediatric patients are infants and children up to 18 years of age, excluding newborn infants. In contrast, PBLS guidelines apply to infants and children without signs of puberty.119
Additions to PALS recommendations include post–cardiac arrest care, neuroprognostication, and recovery. This 2025 summary focuses solely on PALS and highlights new and updated recommendations that will have important impacts on process and patient-related outcomes from cardiac arrest. Additional pediatric-specific guidance and recommendations are provided for PBLS in “Part 6: Pediatric Basic Life Support,”92 recommendations about the training of resuscitation professionals in “Part 12: Resuscitation Education Science,”120 recommendations about SOC in “Part 4: Systems of Care,”40 recommendations for special circumstances in “Part 10: Adult and Pediatric Special Circumstances of Resuscitation,”13 and considerations around ethics in “Part 3: Ethics.”39
Significant New and Update Recommendations
Early Epinephrine
The goal of epinephrine administration during CPR is to optimize coronary perfusion pressure and maintain cerebral perfusion pressure. Earlier administration of epinephrine during CPR is associated with favorable outcomes for infants and children. For infants and children in cardiac arrest with initial nonshockable rhythm, it is reasonable to administer the initial dose of epinephrine as early as possible (COR 2a, LOE C-LD).121-126 Similarly, for infants and children in cardiac arrest with initial shockable rhythm, it may be reasonable to administer epinephrine after 2 attempts at defibrillation or sooner if rapid defibrillation is not possible (COR 2b, C-LD).127,128
Diastolic Blood Pressure to Guide CPR
For patients with continuous invasive arterial blood pressure monitoring in place at the time of cardiac arrest, it is reasonable for health care professionals to use diastolic blood pressure to assess the child’s response to resuscitation efforts (COR 2a, LOE B-NR).129-131 Ideal blood pressure targets during CPR are now provided for infants and children with continuous invasive arterial blood pressure monitoring in place during CPR. In these cases, it may be reasonable for health care professionals to target a diastolic blood pressure ≥25 mm Hg in infants and ≥30 mm Hg in children ≥1 year of age (COR 2b, LOE C-LD).129-131
Post–Cardiac Arrest Blood Pressure Monitoring and Targets
Hypotension is common following resuscitation from cardiac arrest in infants and children and can exacerbate brain and myocardial ischemic injury. Post–cardiac arrest hypotension has been associated with lower rates of survival to hospital discharge. After cardiac arrest in infants and children, continuous arterial pressure monitoring is recommended to identify and treat hypotension when appropriate resources are available (COR 1, LOE C-EO).132-138 In addition, after cardiac arrest in infants and children, it is recommended to maintain systolic and mean arterial blood pressure ≥10th percentile for age (COR 1, LOE B-NR).132-138
Neuroprognostication
Early and reliable neurological prognostication after resuscitation from pediatric cardiac arrest is essential to guide treatment, enable accurate counseling, and provide family support. In addition, accurate neurological prognostication is critical to avoid inappropriate withdrawal of life-sustaining therapy in patients who may have a meaningful recovery, while also avoiding life-sustaining treatments in cases of futility.
Health care professionals are instructed to avoid using single data elements (exam findings such as pupillary light reflex or Glasgow Coma Scale, biomarker, EEG, or magnetic resonance imaging finding) at any given time point to predict good or poor neurologic outcome. Multiple data points are needed to accurately access prognosis for pediatric cardiac arrest survivors (COR 1, LOE B-NR).133,139-151
Knowledge Gaps
Some of the most pertinent gaps in PALS research include the following:
- What is the appropriate age and setting to transition from (1) neonatal resuscitation protocols to pediatric resuscitation protocols and (2) from pediatric resuscitation protocols to adult resuscitation protocols?
- What is the optimal method to transition from weight-based dosing to fixed-dose medication administration during cardiac arrest in adolescents or children with high body mass index?
- With what frequency should doses of epinephrine be administered after the initial dose?
- Should epinephrine dosing strategies be individualized to patients based on hemodynamic response or blood pressure targets?
- Are there specific situations in which advanced airway placement is either beneficial or harmful in OHCA or IHCA? Do they differ based on the etiology of cardiac arrest?
- Can echocardiography or cerebral monitoring improve CPR quality or outcomes from cardiac arrest?
- What is the role of ECPR for infants and children with OHCA and IHCA due to noncardiac causes?
- What is the optimal timing and dosing of initial defibrillation for VF or pulseless VT or subsequent defibrillation for refractory VF or pulseless VT?
- What clinical tools can be used to help in the decision to terminate pediatric IHCA and OHCA resuscitation?
- How can postarrest prognostication be improved with current modalities or new modalities?
- What rehabilitation therapies and follow-up should be provided to improve outcomes after cardiac arrest?
- What are the most effective and safe medications for adenosine-refractory supraventricular tachycardia?
- Are there specific modifications to the cardiac arrest algorithm that should be used when treating a patient with specific conditions, such as myocarditis, cardiomyopathies, single-ventricle congenital heart disease, or pulmonary hypertension?
Adult Advanced Life Support
Part 9 of the 2025 Guidelines, “Adult Advanced Life Support,” includes recommendations for the treatment of adult cardiac emergencies, including immediate arrhythmia management in stable and unstable patients.152 These recommendations are also inclusive of, and have updated upon, the 2023 AHA Focused Update on Adult Advanced Life Support.153 When those arrhythmias result in OHCA or IHCA, these Guidelines also review and recommend the appropriate electrical, medical, and airway management and when and how to consider terminating resuscitation if ROSC is not achieved.
This chapter does not encompass recommendations for BLS, the training of responding health care professionals, special circumstances regarding the provision of advanced life support (ALS) care, post–cardiac arrest care, or the incorporation of ALS techniques or personnel into a resuscitation system of care.24, 154 These topics are each addressed in their own chapters to provide the appropriate attention to those recommendations and the volume of literature analyzed (“Part 2: Evidence Evaluation and Guidelines Development,”21 “Part 4: Systems of Care,”41 “Part 5: Neonatal Resuscitation,”78 “Part 6: Pediatric Basic Life Support,”92 “Part 7: Adult Basic Life Support,”114 “Part 8: Pediatric Advanced Life Support,”118 “Part 10: Adult and Pediatric Special Circumstances of Resuscitation,”13 “Part 11: Post–Cardiac Arrest Care,”155 “Part 12: Resuscitation Education Science”).120 Additionally, considerations around ethics of resuscitation are provided in “Part 3: Ethics.”39
Significant New and Update Recommendations
Cardioversion of Atrial Fibrillation or Flutter
Uncontrolled tachycardia resulting from atrial fibrillation or flutter increases myocardial oxygen demand while simultaneously impairing compensatory measures (ie, ventricular filling, cardiac output, coronary perfusion) to meet that demand. Patients who are unstable and those with rate-related ischemia caused by atrial fibrillation or flutter should undergo urgent electrical cardioversion (COR 1, LOE C-LD). Previous editions of these Guidelines advocated for an incremental approach (using a low initial energy setting and escalating until success); however, it is now recommended to begin at 200 J because new evidence demonstrates greater initial shock success, reduced likelihood of inducing VF, shorter duration of anesthesia (if appropriate), and a smaller cumulative electrical burden with this approach (COR 2b, LOE C-LD).156
Double Sequential Defibrillation
Combined with CPR, successful biphasic defibrillation, creating current across the thorax from electrode pad to pad, is ≈75% effective in terminating VF and VT.157 Double sequential defibrillation has emerged as a potential treatment for those patients with shock-refractory VF.158 Technology to reliably identify shock-refractory VF, in contrast to recurrent VF following defibrillation, and precisely deliver double sequential external defibrillation in the optimal therapeutic window, defined in milliseconds, requires further investigation before being recommended for routine practice (COR 2b, LOE B-R).
Head-Up CPR
Head-up CPR seeks to augment conventional supine CPR to increase cerebral perfusion pressure with the goal of improving favorable neurological outcome.159 Head-up CPR is a bundle of care studied as a combination of mechanical chest compressions, an impedance threshold device, and application of an automated device to control sequential elevation of the head and thorax during compressions.160 Current evidence regarding head-up CPR is limited, and in the absence of RCTs or evaluations with contemporary comparisons, its use is not recommended outside of well-designed clinical trials with the appropriate community consent (COR 3 No Benefit, LOE C-LD).
Polymorphic Ventricular Tachycardia
Sustained polymorphic VT results in reduced ventricular filling and eventual cessation of cardiac output and coronary perfusion, inevitably rendering the patient clinically unstable. While previous editions of these Guidelines have suggested multiple treatment modalities on the basis of clinical stability, it is now recommended that all adult patients with sustained polymorphic VT receive immediate defibrillation (COR 1, LOE B-NR). While other medical treatments may be useful in preventing polymorphic VT or its recurrence on the basis of the underlying pathology (ie, prolonged QT interval; COR 2b, LOE C-LD), these modalities should not delay defibrillation to terminate polymorphic VT.
Knowledge Gaps
Some of the most pertinent gaps in adult ALS research include the following:
- How can technologies developed to diagnose the underlying cardiac rhythm during CPR be used to guide patient management with ALS techniques (ie, timing or vector of defibrillation, administration of epinephrine)?
- How can echocardiography, independent of method (transthoracic or transesophageal), augment the performance of CPR and outcomes from cardiac arrest?
- What is the optimal application of termination of resuscitation guidelines on the basis of the makeup of the responding EMS agency?
- What is the optimal dosing, timing, and route of delivery for epinephrine to maximize neurologically intact survival?
- How should ALS techniques, or the order of their performance, change in the setting of OHCA or IHCA in an adult with congenital heart disease?
- What are the most effective and safe methods for termination of adenosine-refractory supraventricular tachycardia?
- What is the best method to incorporate measures of acute physiology (end-tidal carbon dioxide, arterial blood pressure, etc) into resuscitation decision-making, including the consideration of terminating efforts?
- How do alternative positions for CPR (head-up CPR, etc) affect or improve its performance and the subsequent outcomes (ROSC, neurologically intact survival)?
- Are there specific situations or health care professional characteristics in which the choice of advanced airway placement is either beneficial or harmful in OHCA or IHCA? Do they differ based on the etiology of cardiac arrest?
- What is the role of noninvasive methods of aortic occlusion in successful resuscitation from cardiac arrest?
Adult and Pediatric Special Circumstances of Resuscitation
Part 10 of the 2025 Guidelines, “Adult and Pediatric Special Circumstances of Resuscitation,” includes modifications to basic and advanced life support for adults and children in special situations.13 Depending on the data available, recommendations are made for the management of patients in cardiac arrest or for patients with life-threatening conditions inclusive of cardiac arrest. In the 2020 Guidelines, special circumstances of resuscitation were included within the recommendations for adult basic and advanced life support.24 For the 2025 Guidelines, we emphasized the review of evidence for both the adult and pediatric populations and provided recommendations for the population where applicable. Adult and pediatric recommendations were provided concurrently when the COR and LOE aligned, and, otherwise, pediatric recommendations were separately provided.
These recommendations are also inclusive of, and have updated upon, the 2023 AHA toxicology focused update161 and the 2024 AHA drowning focused update.162 Additionally, new recommendations were provided for the following topics: interposed abdominal compression, electrocution, gas embolism, high-consequence respiratory pathogens, hyperthermia, durable left ventricular assist device (LVAD), amniotic fluid embolism in peripartum patients, and poisoning following volatile hydrocarbon exposure. In all, the updated special circumstances of resuscitation modified 44 recommendations and added 140 new recommendations (many of which were pediatric specific).
Significant New and Update Recommendations
Extracorporeal Life Support
While not available in every setting or generalizable to undifferentiated cardiac arrest, adults and children in cardiac arrest or a periarrest state with a potentially reversible etiology are being supported with extracorporeal life support devices, such as venoarterial extracorporeal membrane oxygenation in situations such as anaphylaxis (adults and children: COR 2a, LOE C-EO), asthma (adults and children: COR 2a, LOE C-LD), cardiac surgery (adults: COR 2a, LOE C-EO; children: COR 2a, LOE C-LD), cardiac interventional laboratory (adults: COR 2a, LOE C-LD), hypothermia (adults: COR 2a, LOE B-NR; children: COR 2a, LOE C-LD), pregnancy (COR 2a, LOE B-NR), and pulmonary embolism (adults: COR 2a, LOE B-NR; children: COR 2a, LOE C-LD) and in poisonings by agents such as β-blockers, calcium channel blockers, cocaine, local anesthetics, sodium channel blockers, and sympathomimetics. Refer to the guideline for individual COR and LOE for extracorporeal life support use in each of the poisoning agents in adults and children.
High-Consequence Respiratory Pathogen
Chest compressions, bag-mask ventilation, defibrillation, suctioning, and endotracheal intubation should be considered aerosol-generating procedures that pose a risk of infection to resuscitation team members (COR 1, LOE C-LD).163-169 However, a real-world study found that rates of SARS-CoV-2 transmission to resuscitation team members with personal protective equipment were low.170
Hyperkalemia
Clinical evidence supporting IV calcium (adults and children: COR 2b, LOE C-LD) or IV sodium bicarbonate (adults and children: COR 2b, LOE C-EO) administration are limited in humans and uncertain to improve survival or favorable neurological outcomes.171,172 The utility of other therapies such as insulin and glucose (adults and children: COR 2b, LOE C-EO) and inhaled β-agonist (adults and children: COR 3 No Benefit, LOE C-EO), intended to lower potassium concentrations in the setting of cardiac arrest, is unclear when weighing the possible benefits against the risk of harm if potentially interrupting well-established interventions like CPR.171,172
Hyperthermia
Adults and children with life-threatening hyperthermia from environmental causes (adults and children: COR 1, LOE C-EO), cocaine poisoning (adults: COR 1, LOE C-LD; children: COR 1, LOE C-EO), or sympathomimetic poisoning (adults: COR 1, LOE C-LD; children: COR 1, LOE C-EO) should be rapidly cooled, ideally at a rate of at least 0.15 °C/min (adults: COR 2a, LOE C-LD; children: COR 2a, LOE C-EO).173 This is best achieved with immersion in ice water (adults: COR 2a, LOE B-R; children: COR 2a, LOE C-EO).174
Left Ventricular Assist Device
The absence of a palpable pulse can make confirming cardiac arrest in adults and children with an LVAD difficult, so assess perfusion by surrogate markers such as cool skin temperature, central cyanosis, poor capillary refill, and a low mean arterial pressure.175 Treatment includes prioritization of CPR (adults and children: COR 1, LOE C-LD) while simultaneously assessing and attempting to restart LVAD function if a second rescuer is available (adults and children: COR 2b, LOE C-LD).
Pregnancy
Management of cardiac arrest during pregnancy is a complex clinical scenario that requires resuscitation strategies that accommodate the physiological changes of pregnancy.176-178 Manual left lateral uterine displacement during chest compression should be provided for a pregnant cardiac arrest patient when the fundal height is at or above the umbilicus to allow for optimal cardiac output by relieving the compression on the inferior vena cava and aorta (COR 1, LOE C-LD).179 Anatomic and physiologic changes of pregnancy add difficulty to airway management given the lack of tolerance for hypoxia and risk of aspiration. Airway management should be prioritized during the resuscitation of a pregnant patient in cardiac arrest (COR 1, LOE C-LD).177 Resuscitative delivery relieves aortocaval compression and returns sequestered uterine blood back to the systemic circulation in efforts to resuscitate the pregnant patient. Team preparation should begin at the recognition of cardiac arrest, and delivery of the fetus should be complete by 5 minutes (COR 1, LOE B-NR).177
Opioids
For trained rescuers assisting an adult or child with suspected opioid overdose who has respiratory depression or respiratory arrest and has a definite pulse, breaths or bag-mask ventilation should be provided (COR 1, LOE B-NR). For lay rescuers assisting an adult or child with suspected opioid overdose who is unresponsive and not breathing normally, CPR with breaths should be provided (COR 1, LOE B-NR). An opioid antagonist (eg, naloxone) should be given to people with respiratory arrest from suspected opioid overdose (COR 1, LOE B-NR). Trained rescuers, lay rescuers, and members of the general public can all administer naloxone.
Knowledge Gaps
Some of the most pertinent knowledge gaps in adult and pediatric special circumstances include the following:
- Does a higher dose of epinephrine, such as 5 mg administered intramuscularly in adults, confer benefit in cardiac arrest from anaphylaxis?
- Is there survival benefit to the use of intracoronary epinephrine to treat adult cardiac arrest in the cardiac intervention laboratory?
- Is there a benefit to 3 stacked shocks in VF in adults after cardiac surgery compared with standard measures for ALS?
- How does resuscitation using airway-breathing-compressions versus compressions-airway-breathing affect outcomes in cardiac arrest following drowning?
- Is drying the chest before using an AED on a drowned child or adult necessary for safe defibrillation, and does it improve rates of success?
- How can teams mitigate the effects of personal protective equipment on resuscitation team performance and health care professional fatigue?
- What is the benefit or harm of calcium in the treatment of hyperkalemia and cardiac arrest?
- In adults and children with cardiac arrest due to environmental hypothermia, what is the optimal temperature to rewarm to prior to defibrillation and administration of epinephrine?
- What is the best method to confirm cardiac arrest in an adult or child with an LVAD?
- What is the optimal airway management device and timing in cardiac arrest in pregnancy?
- What is the optimal amount of time chest compressions should be continued after patients in cardiac arrest from pulmonary embolism receive systemic fibrinolytics?
- Does high-dose insulin therapy for adults and children with life-threatening β-blocker or calcium channel blocker poisoning, administered in addition to or instead of standard vasopressors, reduce mortality or ischemic complications?
- What is the benefit of naloxone when given to adults and children in cardiac arrest with suspected opioid overdose?
Post-Cardiac Arrest Care
Post Cardiac Arrest Care Part 11 of the 2025 Guidelines, “Post–Cardiac Arrest Care,” includes recommendations for the care of adult patients after ROSC.155 These recommendations are also inclusive of, and have updated upon, the 2023 AHA adult life support focused update.153 This encompasses management in the prehospital, emergency department, and in-hospital settings. The management of patients in the post-ROSC period is critically important and spans the Chain of Survival from the acute resuscitation period through survivorship. These Guidelines contain recommendations for post–cardiac arrest care that are based on the best available resuscitation science. This summary highlights new and updated recommendations that may improve outcomes from cardiac arrest.
Significant New and Update Recommendations
Post-ROSC Diagnostics
Twelve-lead electrocardiogram, echocardiography, point-of-care cardiac ultrasound, and computed tomographic imaging are used in postarrest patients to identify clinically significant diagnoses requiring intervention, including evaluating for the underlying cause of cardiac arrest as well as identification and treatment of complications from cardiac arrest and CPR. A 12-lead electrocardiogram should be performed (COR 1, LOE B-NR), and it may be reasonable to perform computed tomography (COR 2b, LOE B-NR), echocardiography (COR 2b, LOE C-LD), or point-of-care cardiac ultrasound (COR 2b, LOE C-LD) for adult patients after ROSC. The use of these diagnostic modalities is reviewed, and the recommendations regarding ultrasound and computed tomographic imaging are new additions.
Duration of Temperature Control
Temperature control refers to the entire period of active temperature management, either to a hypothermic or normothermic target. Maintaining a temperature between 32 °C and 37.5 °C in patients unresponsive to verbal commands after ROSC is recommended for adults (COR 1, LOE B-R). In settings where a hypothermic target is used initially, a period of fever prevention or temperature control to a normothermic target may follow. Trials are heterogeneous in their durations of temperature control, for both hypothermic and normothermic targets. One RCT found no difference in outcomes comparing hypothermic temperature control for 24 hours versus 48 hours.190 Another RCT found no difference in outcomes comparing a period of device-based fever prevention of 12 hours versus 48 hours after an initial 24-hour period of temperature control to 36 °C (36 hours versus 72 total hours of temperature control).181 Other RCTs protocolized all patients to 72 hours of total temperature control.182,183 Recognizing evolution of evidence and definitions with respect to temperature control, 36 hours of total temperature control is the shortest recommended duration (COR 2a, LOE B-R).
Management of Post-ROSC Shock
Hypotension requiring vasopressors is common in post-cardiac arrest patients.184,185 There are no large-scale RCTs comparing clinical outcomes between different vasopressors. Data from patients in cardiogenic shock, many of whom experienced cardiac arrest, suggest epinephrine and dopamine have been associated with a less favorable safety profile; however, this was not found in a recent meta-analysis of the literature focused on cardiac arrest patients.186-188 Thus there is insufficient evidence to recommend a specific vasopressor to treat low blood pressure in adult patients after cardiac arrest (COR 2b, LOE B-NR). Additionally, temporary mechanical circulatory support devices have been used to increase blood pressure and cardiac output in patients with cardiogenic shock, often as an adjunct to vasopressor therapy. In highly selected adult patients with refractory cardiogenic shock after cardiac arrest and ROSC, temporary mechanical circulatory support may be considered (COR 2b, LOE B-NR).
Invasive Neuromonitoring
Hypoxic-ischemic brain injury leads to disruptions in the physiological processes involved in cerebral homeostasis, leading to risks of secondary brain injury.189 Neurologic injury is the primary cause of death in patients who initially survive to ROSC; thus, there is interest in improving neurologic care in the postarrest period. While several studies have examined different approaches to invasive neurologic monitoring for hypoxic-ischemic brain injury, methodological limitations exist that limit the ability to make a recommendation about any invasive neuromonitoring technique. A discussion on the usefulness of monitoring intracranial pressure, cerebral blood flow, and brain tissue oxygenation was included in the Guidelines, acknowledging the growing body of literature on this topic and the movement toward personalized neurologic care in the post–cardiac arrest period. The usefulness of these different invasive neuromonitoring modalities has not been established (COR 2b, LOE C-LD).
Management of Seizures and Myoclonus
Seizures and status epilepticus are common acute neurologic complications in the post–cardiac arrest period, occurring in 10% to 35% of patients who do not follow commands after ROSC.190-195 Myoclonus is a clinical exam finding that may be a manifestation of a seizure if it occurs time locked with an EEG correlate, or myoclonus may occur without an EEG correlate. Thus, after ROSC, promptly performing and interpreting an EEG is recommended for the diagnosis of seizures in adult patients with myoclonus (COR 1, LOE C-LD). Recommendations addressing diagnosis and management of myoclonus and management of EEG findings on the ictal-interictal continuum are important additions.
Neuroprognostication for Favorable Outcome
Accurate neuroprognostication is important to avoid inappropriate withdrawal of life support in patients who may otherwise achieve a favorable outcome and to avoid ineffective treatment when an unacceptable or unfavorable outcome is inevitable.196 Neuroprognostication has historically focused on identifying prognostic tests that predict unfavorable outcome with high specificity. There is increasing focus on developing prognostic tests that predict favorable outcome. Recommendations focused on prognosis for favorable outcome are new additions to these Guidelines.
Health Care Professional Burnout
An important addition to the Guidelines is acknowledging the stressors placed on health care professionals who care for patients with cardiac arrest.
Burnout among health care workers is common197 and negatively impacts health care professionals’ productivity (eg, absenteeism, turnover)198 and patient care (eg, reduced patient satisfaction, increased errors by health care professionals).199 Randomized controlled trials targeting burnout in health care workers have led to some improvement in at least one dimension of burnout or mental health outcome.200-206 Variability in intervention methods and outcome measures, considerable attrition, and high risk of bias inherent in behavioral trials limit the degree to which any one well-being intervention method can be recommended. Nonetheless, interventions to address health care professional burnout may be beneficial (COR 2b, LOE B-NR).
Knowledge Gaps
Questions that address some of the most pertinent knowledge gaps in post–cardiac arrest care include the following:
- How does one select target temperature?
- What is the optimal timing for initiation and duration of temperature control?
- Should the approach to temperature control vary based on patient characteristics?
- Is there a preferred method of cooling and rewarming?
- How does one select physiologic targets (blood pressure, oxygenation, ventilation, etc) for individual patients in the postarrest period?
- How does one achieve optimal physiologic targets in the postarrest period (eg, vasopressor selection, role of mechanical circulatory support, role of intracranial monitoring)?
- Do subgroups of patients (eg, chronic lung disease, immunocompromised status) benefit from early antibiotic administration after ROSC?
- What is the optimal combination of prognostic tests (eg, clinical examination in combination with neuroimaging or EEG to predict outcome)?
- What is the optimal timing for obtaining prognostic tests?
- What are threshold cutoffs that predict unfavorable outcome?
- How can prediction of favorable outcome be improved?
- How can future neuroprognostication research mitigate biases introduced from withdrawal of life-sustaining treatment?
- When is the optimal time to assess survivors and caregivers for emotional distress?
- What are optimal components of psychosocial interventions to address survivor and caregiver emotional distress?
- What are optimal interventions to address burnout in health care professionals?
Resuscitation Education Science
Part 12 of the 2025 Guidelines, “Resuscitation Education Science,” includes recommendations about various instructional design features in resuscitation training, including CPR feedback devices, rapid-cycle deliberate practice, scripted debriefing, gamified learning, spaced learning and booster training, teamwork and leadership training, manikin fidelity, virtual and augmented reality, and the use of cognitive aids.120 Recommendations for these instructional design elements have been split into those for health care professionals and those for lay rescuers. The second section of Part 12 describes how specific health care professional considerations may influence the impact of educational interventions, including disparities according to sex, gender, race, socioeconomic status, and language as well as factors that act as barriers or facilitators to lay rescuer willingness to perform CPR.
Significant New and Update Recommendations
Feedback Devices During CPR Training
It is recommended that feedback devices be used during training for health care professionals (COR 1, LOE A) and lay rescuers (COR 1, LOE A). Feedback devices for CPR provide objective, real-time data to learners during training. This is an advantage over visual observation of CPR by an instructor, which has been shown to be unreliable.207-209 A meta-analysis of 17 RCTs among health care professionals found that CPR feedback devices had a moderate to large positive effect on CPR quality metrics. A separate meta-analysis of 3 randomized trials in lay rescuers found that depth and rate compliance were improved.
Disparities in CPR Education
It is recommended to focus and tailor lay rescuer CPR training to specific racial and ethnic populations and neighborhoods and incorporate awareness efforts in the United States (COR 1, LOE B-NR). Cohort studies have shown that residents of Black and Hispanic neighborhoods are less likely to be trained in or to receive CPR.210-215 Additional studies have shown that neighborhood mapping to identify areas for targeted training is feasible.216,217
It is recommended to prioritize low socioeconomic status populations and neighborhoods for lay rescuer CPR training and awareness efforts (COR 1, LOE B-NR). Cohort studies have shown that low socioeconomic status is associated with less CPR training and lower likelihood of receiving lay rescuer CPR.212,218-232
It is recommended to address barriers to lay rescuers performing CPR on females, through educational training and public awareness efforts (COR 1, LOE B-NR). Women are less likely to receive lay rescuer CPR in public places.233,234 Studies of potential lay rescuers have shown prevalent misconceptions about causing injury and concern about being accused of inappropriate contact with people experiencing cardiac arrest.235,236
It is reasonable to address barriers to linguistically isolated communities by increasing availability and access to CPR training materials in diverse languages (COR 2a, LOE C-LD). Language barriers in communities have been associated with lower rates of lay rescuer CPR.237-242
It is reasonable to consider cost-effective methods for CPR training and promoting safe access to CPR training for low socioeconomic status populations and settings (COR 2a, LOE C-LD). Cost, safety concerns, and insufficient information availability are barriers to CPR training in low socioeconomic status neighborhoods.239,241-244
CPR Training in Schoolchildren
It is recommended that children aged 12 through 18 years be trained to perform high-quality CPR (COR 1, LOE C-LD). Multiple studies have shown that children ≥12 years can learn and perform effective chest compressions.245-249
It is recommended to start CPR training children <12 years in order to increase willingness and self-confidence in later years (COR 1, C-LD). Schoolchildren from the age of 4 to 7 years of age can adequately make an emergency call250-255 or follow the instructions of an AED.251-254 Moreover, a playful approach to CPR at early ages promotes motivation and interest in schoolchildren <12 years and annual repetition can increase the willingness and self-confidence related to the initialization of resuscitation measures in later years.255
Virtual and Augmented Reality
It may be reasonable to use virtual reality (VR) to support knowledge acquisition in basic and advanced life support training for lay rescuers and health care professionals (COR 2b, LOE B-R). Virtual reality refers to training with simulated patients via interactive scenarios within 3-dimensional replications of actual care environments. Four studies of VR use in BLS education found better knowledge acquisition than with other forms of training.256-259
Virtual reality should not be used to teach CPR skills in laypeople and health care professionals (COR 3: Harm, LOE B-R). Multiple studies of CPR quality performance comparing VR-based training to standard training found that VR resulted in poorer compliance with guidelines for chest compression depth, rate, and recoil.260-264
The use of augmented reality to provide real-time CPR feedback may be considered for BLS training of laypeople and health care professionals (COR 2b, LOE CL-D). Augmented reality refers to the use of holographic images overlaid onto a real clinical environment. Four RCTs using augmented reality for CPR feedback during training yielded mixed results, with one study showing better overall CPR performance265 and other studies showing no difference.266-268
Gamified Learning
It may be reasonable to use gamified learning elements as a component of resuscitation training for health care professionals (COR 2b, LOE C-LD). Gamified learning involves the use of game-like elements during resuscitation training. These elements can include competition, point systems, scaffolded levels of difficulty, and leaderboards. Gamification has been shown to increase learner engagement and enhance recall of content.269
Scripted Debriefing
It may be reasonable for an instructor to use a debriefing script during resuscitation education (COR 2b, LOE C-LD). Scripted debriefing involves the creation of a written plan for debriefing learners during and following life support training. These scripts aim to standardize debriefing during resuscitation training, supporting facilitators with a clear plan and guiding discussion. Standardized debriefing helps to maintain consistency in the delivery of debriefings across training centers and resuscitation programs. Randomized controlled trials in resuscitation training settings showed that scripted debriefing was associated with improved CPR quality,270 improved team leadership and knowledge acquisition,271 and improved debriefing quality among novice instructors.272
Rapid-Cycle Deliberate Practice
It may be reasonable to incorporate rapid-cycle deliberate practice as part of basic or advanced life support training for health care personnel (COR 2b, LOE C-LD). Rapid-cycle deliberate practice is defined by rapid cycling between deliberate practice and directed feedback until skill mastery is achieved.273 Multiple studies have demonstrated that this training is associated with faster initiation of chest compressions, defibrillation, ventilation, and epinephrine administration, as well as improved compression fraction and shorter pauses before defibrillation.273-277
Alternative Objects for Chest Compression Training Lay Rescuers
The usefulness of alternative objects (as an alternative to a manikin) to train laypeople in chest compressions is not well established (COR 2b, LOE C-LD). Barriers to CPR training in low-resource settings include cost, access to training centers, and time constraints. Studies of low-cost, easy-access objects as an alternative to manikins (eg, pillow, foam blocks, toilet paper, rolls, plastic bottles), which allow lay rescuers in low-resource settings to train in chest compressions, have yielded mixed results.278-284
Knowledge Gaps
Some of the most pertinent gaps in resuscitation education research include the following:
- What are the optimal methods for identifying and targeting areas with lower prevalence of CPR training and lower lay rescuer CPR rates? What methods best overcome barriers to training for people living in those areas?
- Which educational interventions most impact real-world performance and clinical outcomes, as opposed to educational outcomes or performance in training?
- How can instructional design features be combined or blended to optimize outcomes? Future studies should evaluate the synergistic effects of instructional design features when used in a blended manner.
- What are the most effective ways to train and develop resuscitation instructors? Future research should evaluate the impact of various faculty development strategies on instructor skills and learner outcomes.
- What is the impact of varying levels of cost, resource and personnel availability, and training center infrastructure on the ability to implement technology-dependent instructional design features (eg, high-fidelity manikins, VR)?
Cardiac arrest remains a serious condition with high morbidity and mortality, impacting individuals of all ages, sexes. genders, races, geographic regions, and socioeconomic backgrounds. While survival rates have seen some improvements since 2020, substantial efforts are still needed to reduce the significant burden of this disease. This executive summary outlines updated and new recommendations from the 2025 Guidelines, developed through rigorous evidence evaluation, and new horizons of ethical challenges that result from advancing resuscitation science.
Continued progress over the next decade will require strengthening the Chain of Survival and enhancing coordinated SOC. The knowledge gaps identified in the 2025 Guidelines highlight critical research questions that should be addressed, presenting key opportunities for future funding in resuscitation science. While developing Guidelines is a crucial first step, their implementation and ongoing research will be essential in driving meaningful improvements in patient outcomes. Funding for such research is a critical priority in reducing death and disability from cardiac arrest.
The American Heart Association requests that this document be cited as follows: Del Rios M, Bartos JA, Panchal AR, Atkins DL, Cabanas JG, Cao D, Dainty KN, Dezfulian C, Donoghue AJ, Drennan IR, Elmer J, Hirsch KG, Idris AH, Joyner BL, Kamath-Rayne BD, Kleinman ME, Kurz MC, Lasa JJ, Lee HC, McBride ME, Raymond TT, Rittenberger, JC, Schexnayder SM, Szyld E, Topjian A, Wigginton JG, Previdi JK. Part 1: executive summary: 2025 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2025;152(suppl):S284–S312. doi: 10.1161/CIR.0000000000001372
- Marina Del Rios, MD, MS, Chair
- Jason A. Bartos, MD, PhD
- Ashish R. Panchal, MD, PhD
- Dianne Atkins, MD
- José G. Cabañas, MD, MPH
- Dazhe Cao, MD
- Katie N. Dainty, PhD
- Cameron Dezfulian, MD
- Aaron J. Donoghue, MD, MSCE
- Ian R. Drennan, ACP, PhD
- Jonathan Elmer, MD, MS
- Karen G. Hirsch, MD
- Ahamed H. Idris, MD
- Benny L. Joyner, MD, MPH
- Beena D. Kamath-Rayne, MD, MPH
- Monica E. Kleinman, MD
- Michael C. Kurz, MD
- Javier J. Lasa, MD
- Henry C. Lee, MD
- Mary E. McBride, MD, Med
- Tia T. Raymond, MD, MBA
- Jon C. Rittenberger, MD, MS
- Stephen M. Schexnayder, MD
- Edgardo Szyld, MD, MSc
- Alexis Topjian, MD, MSCE
- Jane G. Wigginton, MD, MSCS
- Jeanette K. Previdi, MPH, BSN, RN, Vice Chair
The writing group acknowledges the members of the Evidence Evaluation and Guidelines Development, Ethics, Systems of Care, Neonatal Resuscitation, Pediatric Basic Life Support, Basic Life Support, Pediatric Advanced Life Support, Advanced Life Support, Special Circumstances, Post–Cardiac Arrest Care, and Resuscitation Education Science Writing Groups. We especially would like to thank the following individuals for their contributions: Laura Haygood, MLIS; Chalan King, MS; Melissa Mahgoub, PhD; Peace Ossom, MLS, MS; Abdul Pullattayil, MISt, AHIP; Amber J. Rodriguez, PhD; Comilla Sasson, MD, PhD; Julie Sell, MSN, RN; and Jaylen Wright, PhD.
Disclosures
Open table in a new window.
Open table in a new window.
 Login
Login

